|
Back to Annual Symposium Program
Comparative Analysis of Endovascular and Open Popliteal Artery Aneurysm Repair; Mid-term Results
Melanie R. Hoehn, MD, Ryan M. McEnaney, MD, Theodore H. Yuo, MD, Rabih A. Chaer, MD, Robert Y. Rhee, MD, Michel S. Makaroun, MD, Luke K. Marone, MD.
University of PA-Medical Center, Pittsburgh, PA, USA.
OBJECTIVE: To compare patency of endovascular (ER) and open repair (OR) of popliteal artery aneurysms (PAA) and determine predictors of failed revascularization. The focus is mid-term patency, as only early outcomes of ER are well known.
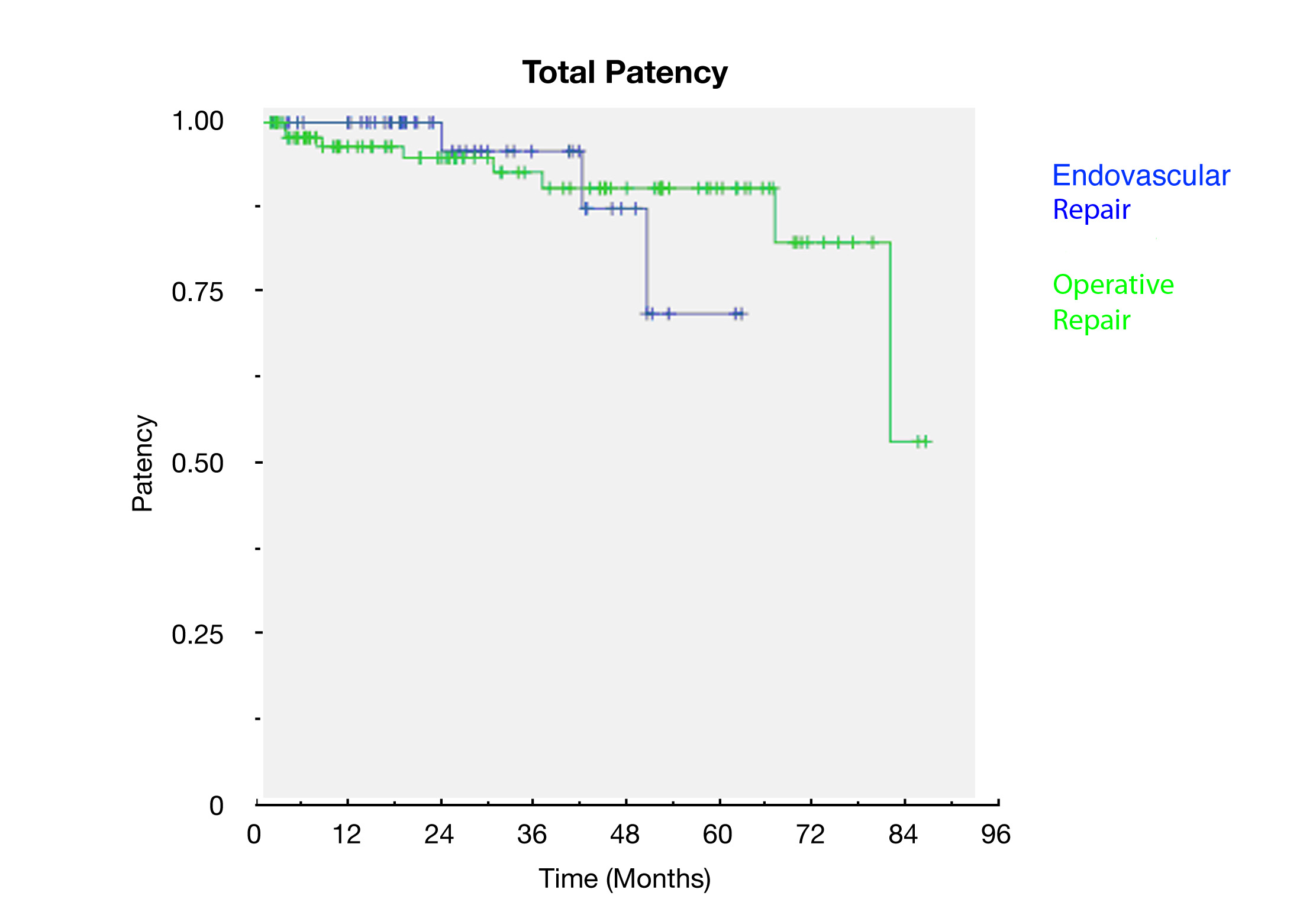
METHODS: A retrospective review of all patients treated for PAA from 2004 -2010 was conducted at one institution. Indications for and details of repair, patient characteristics, and outcomes were reviewed. Kaplan-Meier curves were used to estimate patency rates. Multivariate analysis was performed to determine factors predictive of patency.
RESULTS: A total of 161 PAAs underwent endovascular repair in 50 and open surgical repair in 111 (8.0% and 20.7% emergent respectively p=.067). Follow-up was available for 151 repairs and mean follow-up time was 29.7 (+/-2.4) months. The average age of patients at the time of repair was 70.6 (+/- 12.7) and 96% were male. Of the bypass group, 72.1% were performed with native conduit. Operative mortality was 2.0% for the ER group and 3.6% for the OR group (p=1). ER had a significantly lower complication rate (14.0% vs 32.4% p=.020) and shorter LOS (median 1 vs 4 days p= <.001). Rates of reintervention to maintain patency were similar (12.2% and 10.8% p=.789). Two year primary patency rate was 83.3% for ER, and 80.0% for OR (p=.779); overall patency was 96.7% and 87.3% (p=.250) respectively. There was one amputation in each group, both in the setting of a patent bypass. Overall limb salvage rate was 98.0% with ER and 99.1% with OR (p=.526). SVS runoff scores were significantly better in the bypass group (Mean 9.2 vs 4.8, p=<.01). Univariate analysis revealed plavix (p=.037), and antegrade puncture (p=.048) in the ER group and statin use (p=.027) in the OR group were associated with improved patency. Multivariate analysis revealed only statin use to be protective overall (p=.027).
CONCLUSION: Endovascular and bypass techniques for PAA repair have equivalent mid-term patency, limb salvage and reintervention rates. Endovascular repair is a valid option for patients presenting with favorable runoff scores and is associated with a lower complication rate and shorter hospital length of stay. 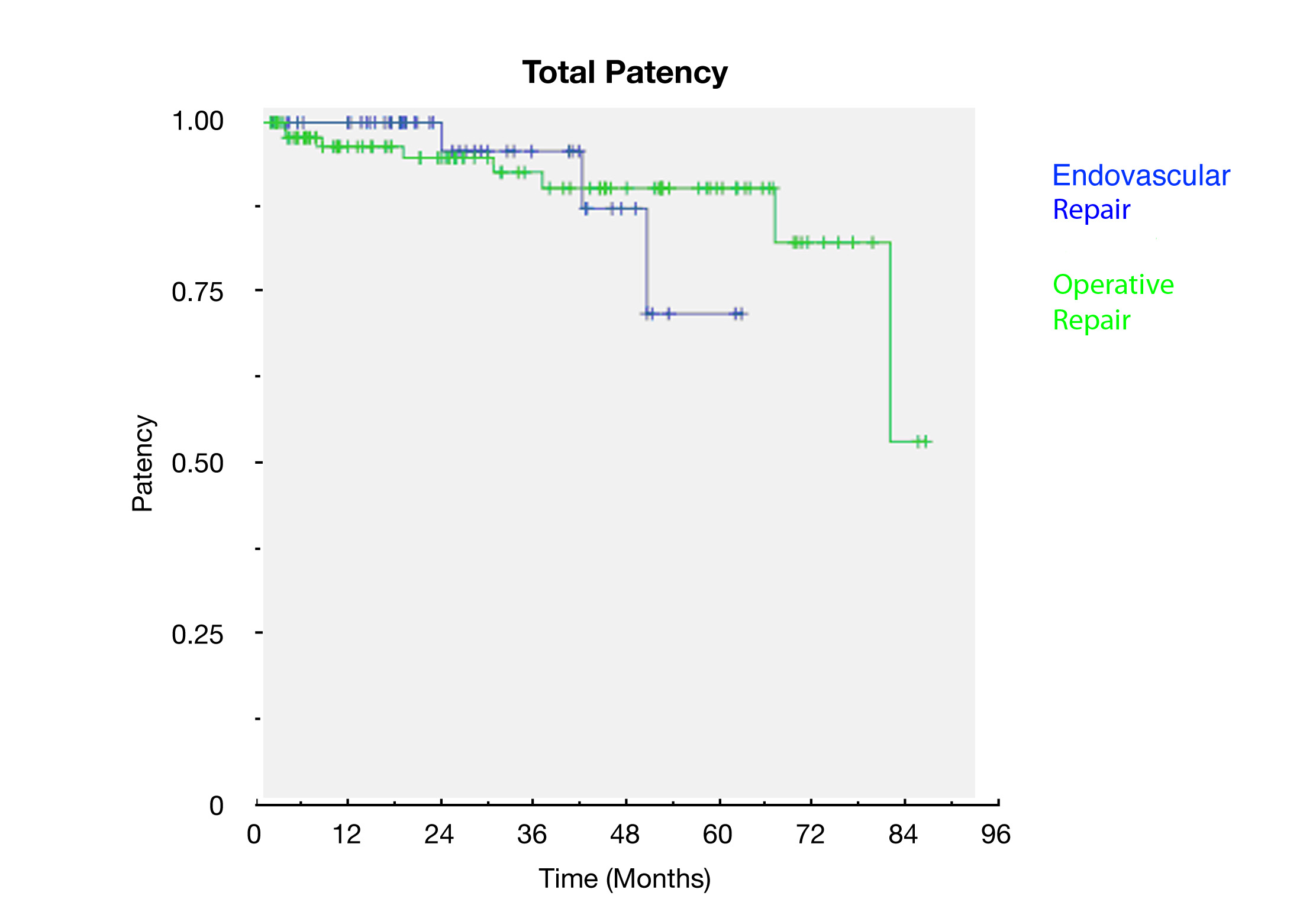
Back to Annual Symposium Program

|