|
|
 |
Back to Annual Symposium Program
Circle of Willis: A major highway for contralateral microemboli during CAS
Kevin Casey, MD1, Elizabeth Hitchner, MA2, Barton Lane, MD3, Weesam K. Al-Khatib, MD3, Wei Zhou, MD3.
1Naval Medical Center San Diego, San Diego, CA, USA, 2Veterans Administration Palo Alto, Palo Alto, CA, USA, 3Veterans Administration Palo Alto, Stanford University Hospital, Palo Alto, Stanford, CA, USA.
OBJECTIVES: Carotid artery stenting (CAS) with distal protection has proven an effective alternative for high-risk patients with severe carotid stenosis. A major concern during CAS is that debris from the aortic arch may travel via either internal carotid artery (ICA) to the cerebrum. Contralateral microemboli are thought to be due to excessive manipulation of a diseased aorta leading to debris embolization via the contralateral ICA. We sought to determine other sources of contralateral microembolization during CAS.
METHODS: Consecutive patients receiving carotid interventions for carotid artery stenosis at a single institution were retrospectively reviewed. Only patients who received both pre- and post- operative MRI with diffusion-weighted sequences (DWI) were included in the study. Patients who had contralateral carotid artery occlusions were the primary focus. The presence of contralateral ICA occlusion, patient characteristics, and anatomic variability were compared.
RESULTS: From 2006-2011, 350 patients underwent carotid interventions. Among them, 247 had pre- and post-procedure MRI evaluations including 23 patients who had contralateral carotid artery occlusions. Fourteen CAS patients (12%) had known contralateral ICA occlusions and 3 patients (21%) demonstrated new contralateral microemboli. All were male, current smokers, and on antihypertensive medications.
One patient had a previous CVA and two patients had a history of atrial fibrillation. One patient developed hemodynamic instability requiring pressor support during the procedure. However, no patient developed symptoms during the procedure or follow-up period. Two patients had a Type II arch, but direct arch embolization to the contralateral hemisphere was unlikely due to contralateral ICA occlusion. All three patients also demonstrated new ipsilateral microemboli.
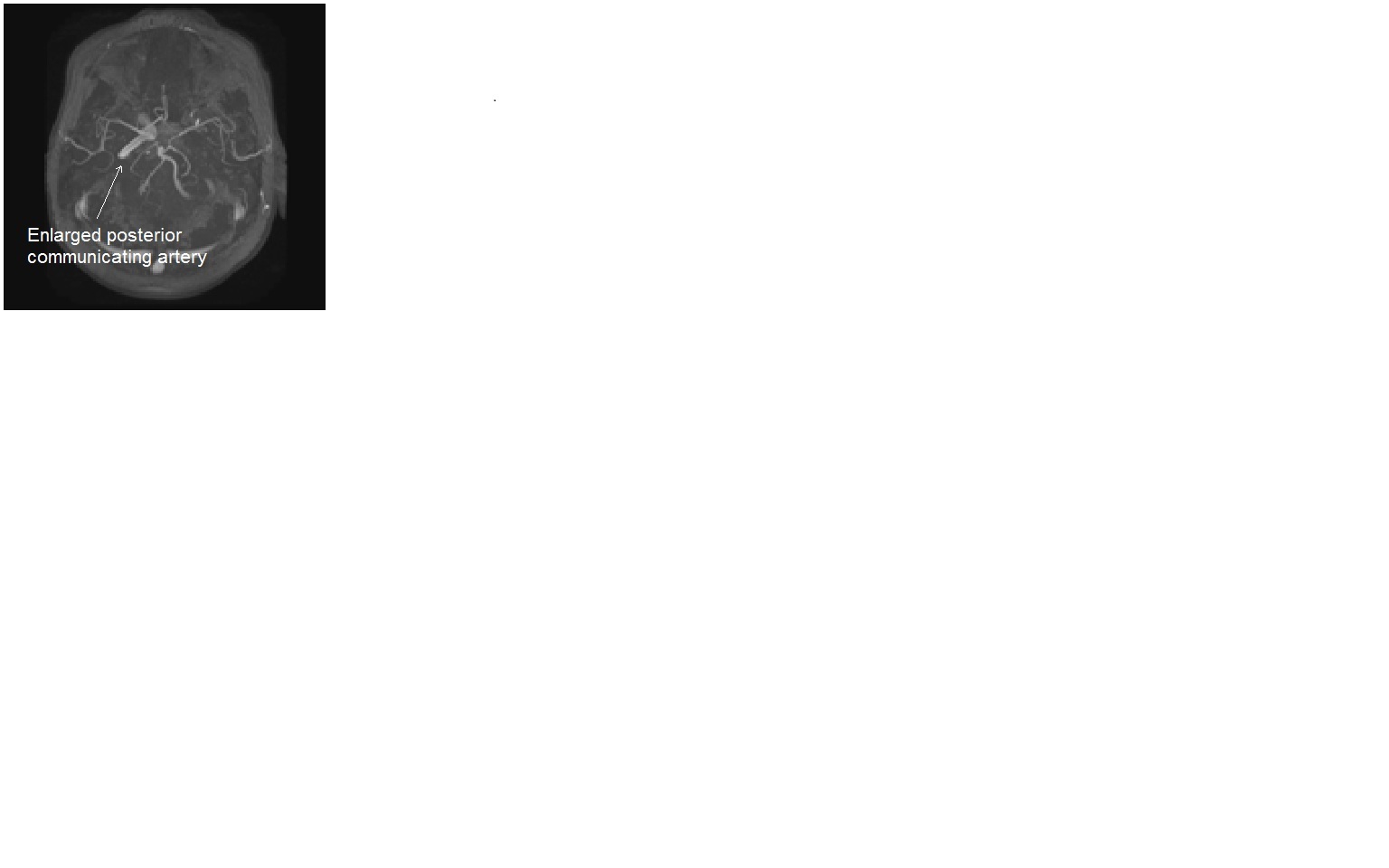
MRI images showed that all patients had a patent Circle of Willis. Two had a very prominent posterior communicating artery, while one patient had a patent anterior communicating artery. Logically, the contralateral DWI lesions originated ipsilaterally and travelled through the intracranial communicating arteries to the contralateral hemisphere.
CONCLUSIONS: Contralateral cerebral embolization during CAS is not a rare occurrence. This series is the first to provide structural evidence of the intracranial primary collateral pathway as an important source of inter-hemispheric microembolization. Larger studies are needed to help predict those patients at greatest risk for contralateral ICA embolization. 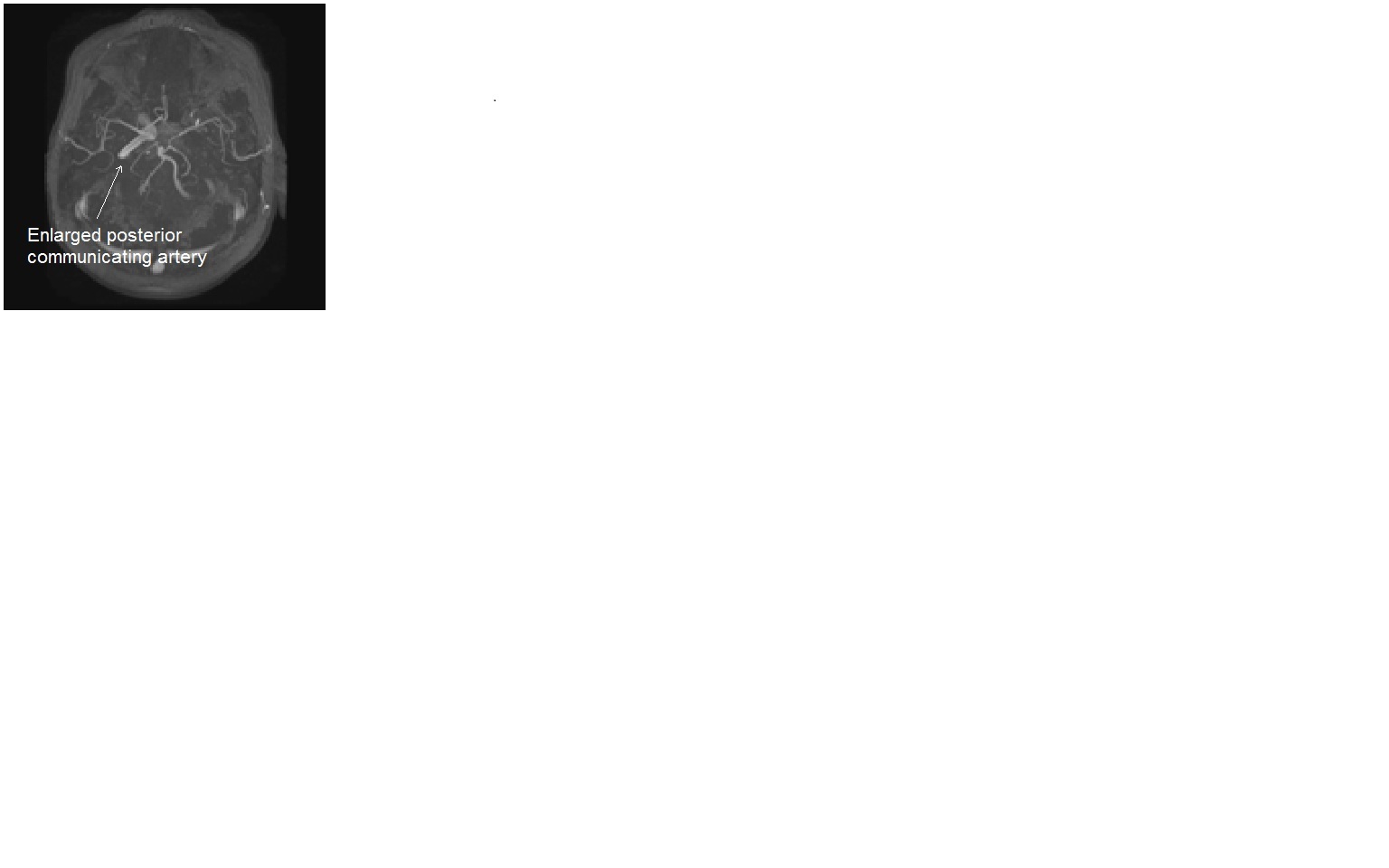
Back to Annual Symposium Program

|