|
Back to Annual Symposium Program
Surgical Bypass or Endovascular Therapy?: How Vascular Surgeons Decide for Patients with Infrainguinal Arterial Disease and Critical Limb Ischemia
Alik Farber1, Gheorghe Doros, PhD2, Matthew Menard, MD3.
1Boston University Medical Center, Boston, MA, USA, 2Boston University School of Public Health, Boston, MA, USA, 3Brigham and Women's Medical Center, Boston, MA, USA.
OBJECTIVES:
The decision to treat critical limb ischemia(CLI) with open surgery(OS) or endovascular therapy(ET) is often guided by individual bias, skill set and intuition rather than established evidence-based criteria. We sought to quantify the degree of equipoise between these treatment options across a range of clinical and anatomic parameters and elucidate the relative importance of these parameters on treatment strategy.
METHODS:
A 123-question survey(multiple choice and Likert scale(1-5)) was administered to vascular surgeons from the United States and Canada recruited to participate in a proposed randomized trial of best OS or ET in patients with infrainguinal arterial disease and CLI. Surgeon demographics(7 questions), open and endovascular experience(25 questions) and surgeon bias(91 questions) were assessed. Treatment equipoise was measured as the sum of individual(personal declaration that equipoise exists) and community(offsetting discordance in choice of competing therapies) equipoise.
RESULTS:
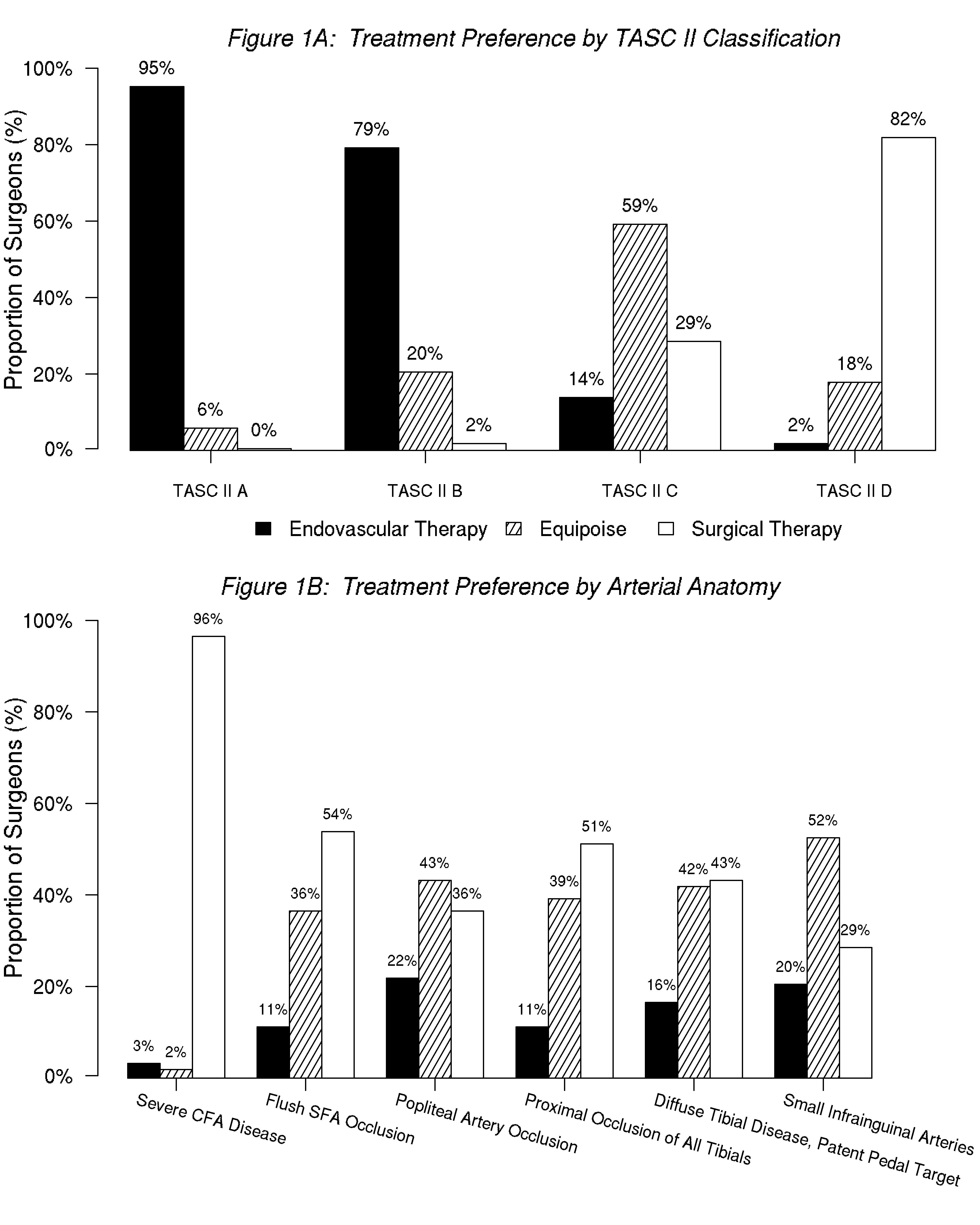
76 of 100 surgeons queried completed the survey. 85% of respondents were academic vascular surgeons, 64% completed training more than 10 years previously and 78% had a OS:ET practice ratio of 40:60, 50:50 or 60:40. Ambulatory status, high surgical risk, severe coronary artery disease, frail appearance, and early surgical failure were judged to be very to extremely important(Likert scale 1 and 2) by 88%, 87%, 87%, 83%, and 80% of respondents in choosing between OS and ET, respectively. A greater degree of treatment equipoise was seen with ischemic rest pain(88%) and minor (92%) than major(58%) tissue loss. 79% of surgeons preferred ET when autogenous vein was unavailable, while treatment equipoise was 49% in the presence of suitable saphenous vein. Treatment equipoise was notably low for TASC D anatomy(Figure 1A). 96% of respondents felt the presence of severe common femoral arterial disease should warrant OS, whereas there was significant equipoise with respect to other anatomical factors(Figure 1B).
CONCLUSIONS:
Our survey identifies significant equipoise across a range of clinical and anatomic variables in the current treatment of CLI within the North American vascular surgery community, and delineates the relative influence of individual clinical and anatomic parameters on the choice of OS or ET. A strong preference for surgical treatment of TASC D lesions was demonstrated. 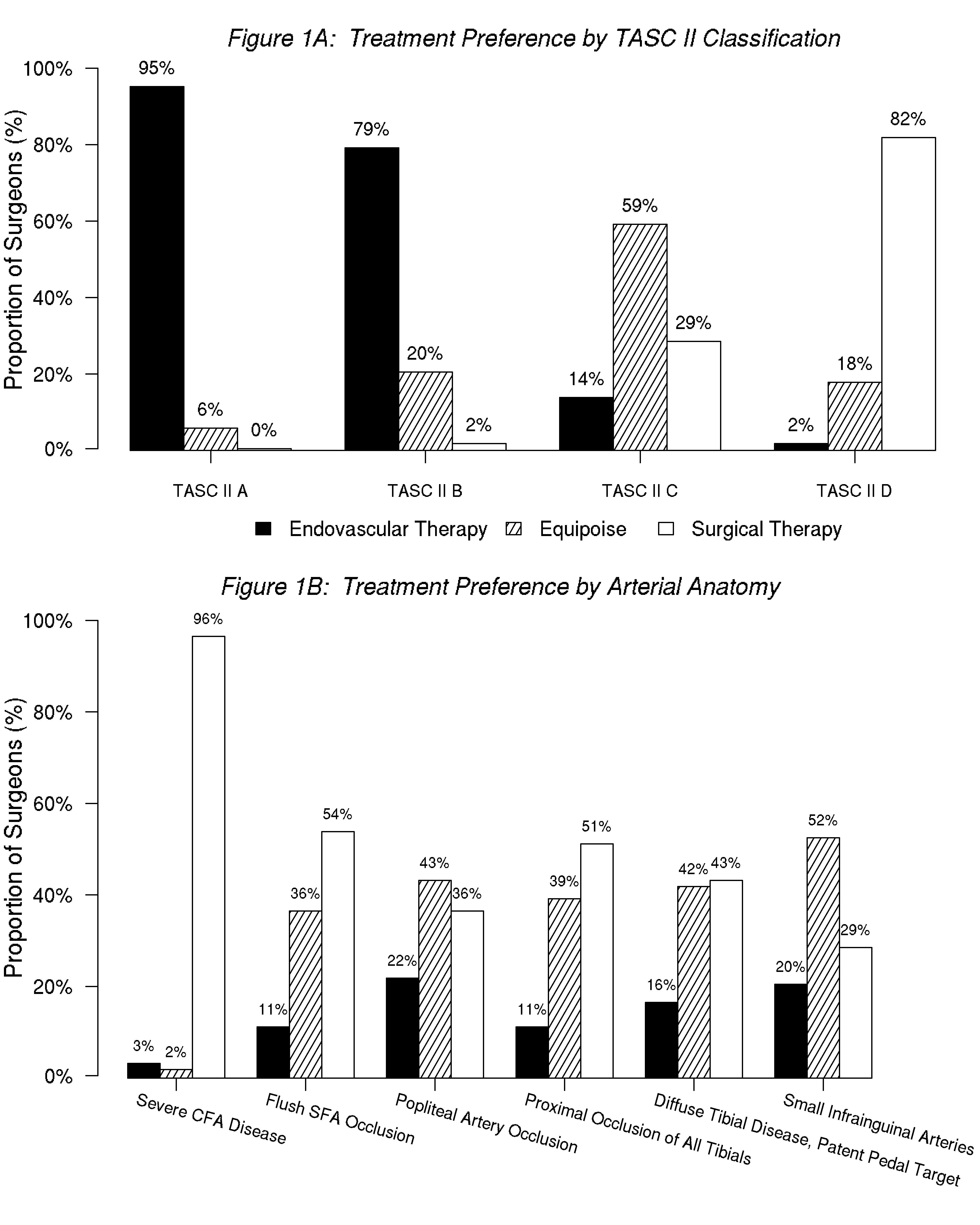
Back to Annual Symposium Program

|