|
Back to Annual Symposium Program
Non-Invasive Quantification of Inter-luminal Pressure Gradient in DeBakey Type B Aortic Dissections
Christof Karmonik, MD, Cassidy A. Duran, MD, Javier E. Anaya-Ayala, MD, Dipan J. Shah, MD, Jean Bismuth, MD, Mark G. Davies, MD, PhD, MBA, Alan B. Lumsden, MD.
Methodist DeBakey Heart & Vascular Center, Houston, TX, USA.
Introduction: Inter-luminal pressure gradient (IPG) the pressure between the true and false lumen in Type B Aortic Dissections (AD) is considered of clinical relevance with highly elevated false lumen to true lumen pressure ratio indicating risk of false lumen expansion and rupture. Non-invasive IPG quantification would be beneficial as invasive pressure catheter measurements pose additional risk to the patient, and may serve as a predictive measure for poor outcome of Type B aortic dissections, which are managed conservatively.
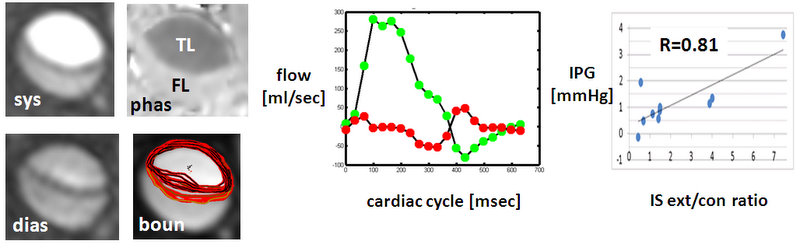
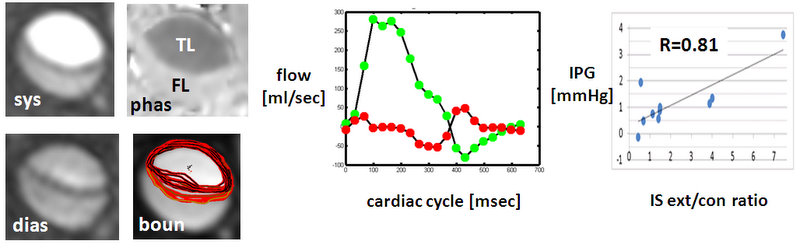
Methods: From 40 AD patients undergoing MRI examinations at the Methodist Acute Aortic Treatment Center, 10 acute AD were selected for further analysis. All examinations included aclinical pcMRI study (figure 1a) from which false lumen and true lumen blood velocities were quantified.Both true and false lumenswere automatically segmented and maximum IS extension and contraction were quantified. IPG was derived by applying the Bernoulli equation. Intra-arterial septum (IS) motion was quantified and correlated with IPG. Pearson correlation coefficientbetween IPG and maximum IS extension, contraction and their ratio was calculated.
Results: In these type B dissections true lumen velocity range was 40 cm/sec to 89 cm/sec (62 ± 16 cm/sec), false lumen velocity was 7 cm/sec to 36 cm/sec (18 ± 11 cm/sec) corresponding to an average static false lumen /true lumen pressure ratio of 11.9 (range: 4.6 to 18.8). IS extension was 2.4 to 5.5 mm (3.5 ± 0.9 mm), IS contraction was 0.8 to 6.9 mm (3.0 ± 1.9 mm). IPG correlated with maximum IS extension (R=0.76) andinversely with maximum IS contraction (R=-0.51).Strength of correlation was highest with IS extension/contraction ratio (R= 0.81, figure 1).
Conclusions: IPG quantified non-invasively with pcMRI strongly correlateswith IS mobility in acute AD. Static false lumenpressures were on average one order of magnitude higher thanthose found in the true lumen. Non-invasive monitoring with pcMRI may be applied at follow-up examinations to correlate false lumen expansion and thrombus formation with IPG.
Back to Annual Symposium Program

|