|
Back to Annual Symposium Program
Endovascular Intervention for Hepatic Artery Stenosis After Liver Transplantation
Blake A. Hamby, MD, Hernan A. Bazan, MD, Taylor A. Smith, MD, Edward Bluth, MD, George E. Loss, MD, Ph.D, W. Charles Sternbergh, III, MD.
Ochsner Clinic Foundation, New Orleans, LA, USA.
OBJECTIVES:
Hepatic artery stenosis (HAS) and thrombosis (HAT) are serious complications of orthotopic liver transplantation (OLT) with 30% risk of graft loss and death. Open vascular reconstruction or re-transplantation are the traditional treatment options. Enhanced collaboration between transplant and vascular services at our institution has provided minimally invasive options for HAS.
METHODS:
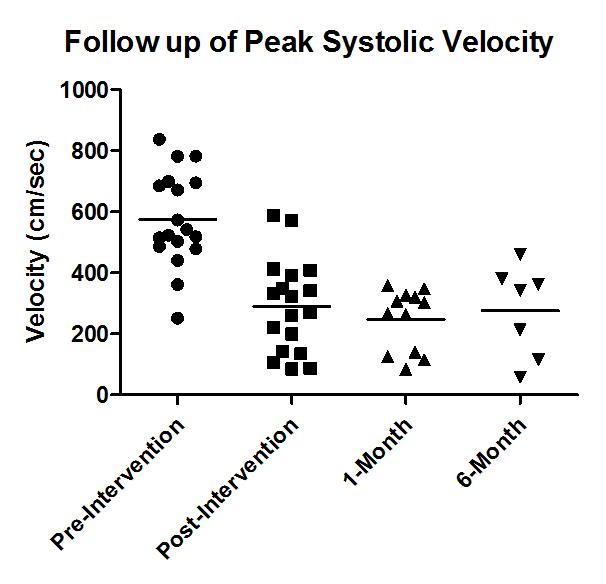
From September 2009 - August 2011, OLT patients with clinical and ultrasound evidence of HAS were evaluated for endovascular treatment. Ultrasound criteria included hepatic artery (HA) peak systolic velocities (PSV) more than triple initial post-transplant evaluation, resistive indices (RI) less than 0.4, and blunted intrahepatic arterial waveforms (tardus parvus). Interventions included percutaneous transluminal angioplasty (PTA) alone or with stent (PTAS). Pre-intervention, post-intervention, one- and six-month follow-up HA velocities and RIs were compared using the two-tailed t-test. Fischer’s exact test compared re-intervention rates.
RESULTS:
Over the study period 237 OLTs were performed with 19 interventions performed in 14 patients with HAS (including 2 previously re-transplanted for HAT), giving an occurrence rate of clinically-significant HAS of 5.9% (14/237). Mean age was 50±8 (range 15-63). Interventions occurred at a mean 82±52 days post-transplant (range 8-233 days). Mean HA velocities before (575±125cm/s) and after (291±123cm/s) intervention significantly improved [p<0.0001], as were mean RIs before (0.41±0.08) and after (0.59±0.08) [p<0.0001]. Mean follow up was 5.7±0.4 months (range 0-23.2). Sustained improvement in PSV and RI was seen for 11 patients with 1-month follow-up (247±87cm/s [p=0.001] and 0.58±0.07 [p<0.0001], respectively) and 7 patients at 6-months (276±126cm/s [p=0.05] and 0.61±0.08 [p<0.0001], respectively). Five patients underwent PTA, of which 3 required re-intervention with PTAS for re-stenosis at a mean of 39 days. From our early experience with early re-stenosis with PTA alone, our policy changed to primary stent placement when technically possible. Nine patients underwent primary PTAS with self-expanding (n=3) or coronary balloon-expandable (n=6) stents. Freedom from re-intervention was 78% with primary stenting versus 40% with PTA[p=0.27]. No treated patient suffered graft loss.
CONCLUSIONS:
Endovascular treatment of HAS after OLT appears safe and effective in the short-term. Primary stenting may provide superior patency compared to PTA alone. Longer follow-up is needed to confirm these early encouraging results. 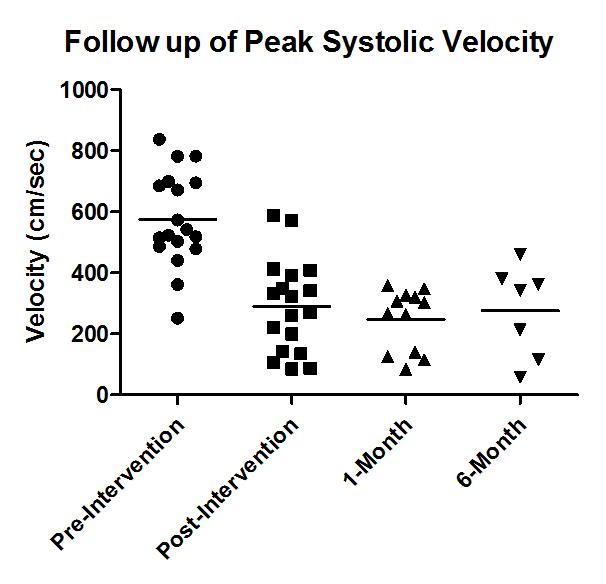
Back to Annual Symposium Program

|