|
Back to Annual Symposium Program
A Single Surgeon and Single Institution Review of Carotid Endarterectomy: Minimal Morbidity and Mortality in a Veteran Population
Daniel Copeland, MD, Sandi Brock, RN, William Stevenson, MS, Mohammed Moursi, MD.
Central Arkansas Veterans Health System, Little Rock, AR, USA.
OBJECTIVES:
Carotid Endarterectomy (CEA) and Carotid Artery Stenting are used in the treatment of extra-cranial carotid stenosis and stroke prevention. This study provides a contemporary cohort of CEA subjects for comparison.
METHODS:
A retrospective review of primary carotid endarterectomies for symptomatic and asymptomatic stenosis was performed at a single Veterans Hospital from 2000- 2010.
RESULTS:
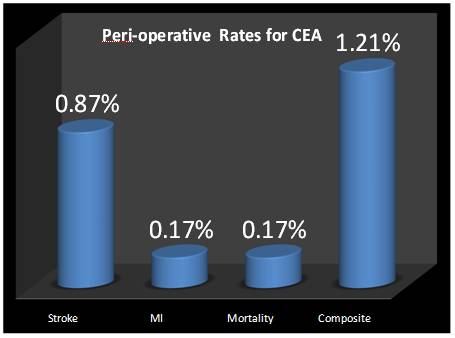
577 veterans were studied. Median age was 67 years with 97% male. 57% were asymptomatic severe stenosis (99%) by ultrasound alone (97%). 98% percent were ambulatory and living independently. Of those who were symptomatic (247), 105(43%) had ocular symptoms, 166(67%) had a transient ischemic attack, and 115(47%) had evidence of an embolic stroke. 79% were on Aspirin alone, 5% on Plavix alone, and 16% on both. Comorbidities included hypertension (83%), coronary artery disease (24%), CHF (11%), diabetes (38%), and peripheral vascular occlusive disease (28%). All surgeries were done under the direction of a single surgeon using a traditional CEA with bovine pericardial patch angioplasty of the internal carotid artery. Fifty-eight percent underwent regional block and 42% general anesthesia. A shunt was utilized in general anesthesia cases and in 11% done under regional block. A vascular fellow was involved in 21% of the cases and a midlevel general surgery resident in 79%. Average operative time was 94 minutes. The average follow up was 50 months with an average length of stay at 3.9 days. The majority were discharged to home ambulatory with independent living status. Few patients were treated for wound infection (1.4%) and seventeen patients (3%) experienced transient nerve dysfunction (16 marginal mandibular, 1 hypoglossal), all resolving within a year. One patient had persistent jaw fatigue. One patient sustained an intraoperative stroke. The thirty-day, one year, and three year stroke rate was 0.87%, 1%, and 1.4% respectively. Two peri-operative strokes were major leading to severe dysfunction and early mortality. The rates for peri-operative myocardial infarction and death rates were both 0.17%. The mortality rate at one year (1.8%), three years (4.8%), and at follow up (12.2%) were also recorded.
CONCLUSIONS:
CEA remains the gold standard for carotid revascularization with low perioperative events in experienced hands. 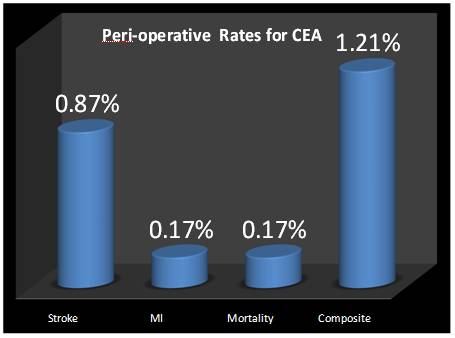
Back to Annual Symposium Program

|