|
Back to Annual Symposium Program
Comparison of Interventional Therapies for Diabetic Ulcers: National Trends from 2001 to 2008
Barbara H. Davis, DO, Justin Lee, MD, Peter Miller, MD, Rocco G. Ciocca, MD.
St. Elizabeth Medical Center, Boston, MA, USA.
Objective
The incidence of hospitalization for diabetes and related wounds increases yearly in the United States. Amputation remains a significant complication of these wounds. With aggressive medical and interventional therapies including endovascular procedures for treating chronic vascular disease in diabetic patients, we hypothesize the rate of lower extremity amputations should be declining. The purpose of this study was to analyze national trends in utilization of various treatment modalities for diabetic ulcers and compare related costs.
Methods
A retrospective analysis of the Nationwide Inpatient Sample (NIS) from 2001 to 2008 was performed. ICD-9 codes were used to identify all diagnoses of diabetic related lower extremity ulcers and surgical procedures used. Using a coding algorithm to identify patients who underwent surgical intervention (amputation, open peripheral bypass, diagnostic angiography, PTA) during admission, national trends were calculated and chronicled.
Results
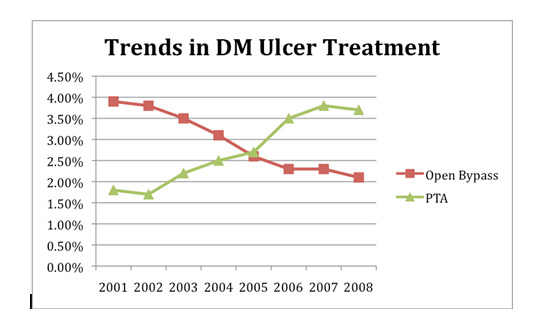
A total of 5,727,764 patients were identified with admitting diagnosis of diabetic lower extremity ulcer during the study period. Mean age was 66.42 (SEM 0.007), 51.2% were males, 49.2% were white, and 66.3% had Medicare coverage. Utilization of open peripheral bypass procedures decreased from 3.9% in 2001 to 2.1% in 2008 (p<0.001). The percentage of patients undergoing angioplasty after diagnostic angiogram increased more than 2-fold, from 20.4% in 2001 to 42.7% in 2008 (p<0.001). Amputation (includes toe, foot, below and above knee) rate remained relatively stable at 11.3%. Comparing amputation to angioplasty, mean total hospital charge was significantly lower with amputation ($53,962.94 versus $74,664.97, p<0.001)). Mean length of stay was also significantly shorter for angioplasty (10.81 days versus 12.81 days, p<0.001).
Conclusions
During the study period, there was significant decrease in peripheral open bypass procedures for patients with diabetic ulcers. The percentage of patients undergoing amputation remained relatively constant despite a corresponding increase in utilization of angioplasty with diagnostic angiography. Although mean length of stay was shorter for angioplasty, there was a significant increase in total hospital charge for these patients. Further studies are needed to determine the role of angioplasty in the ongoing effort to control costs in caring for diabetic patients in the era of shrinking healthcare economic resources. 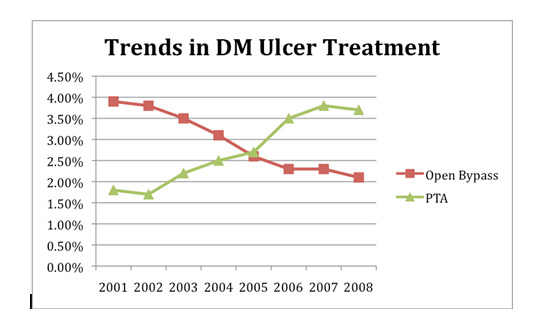
Back to Annual Symposium Program

|