|
Back to Annual Symposium Program
Developing Training Models For Advanced Endovascular Skills: Type II Endoleaks In Abdominal Aortic Aneurysms
Jean Bismuth, MD, Cassidy Duran, MD, Ponraj Chinnadurai, MD, Stephen Igo, Michael A. Donovan, Matthew S. Jackson, Alan B. Lumsden, MD.
The Methodist Hospital/Debakey Heart & Vascular Center/Weill Cornell Medical College, Houston, TX, USA.
Developing Training Models For Advanced Endovascular Skills:
Type II Endoleaks In Abdominal Aortic Aneurysms
Introduction: Endovascular virtual reality simulators provide training in a wide array of endovascular skills, but are not able to provide comprehensive instruction for all vascular procedures. This is particularly the case in procedures that require advanced imaging techniques, tasks that are not strictly endovascular and those that involve new tools. One such skill is Type II endoleak embolization by translumbar approach. Type II embolization was rated by The Society for Vascular Surgery members as one of the most desirable techniques to learn
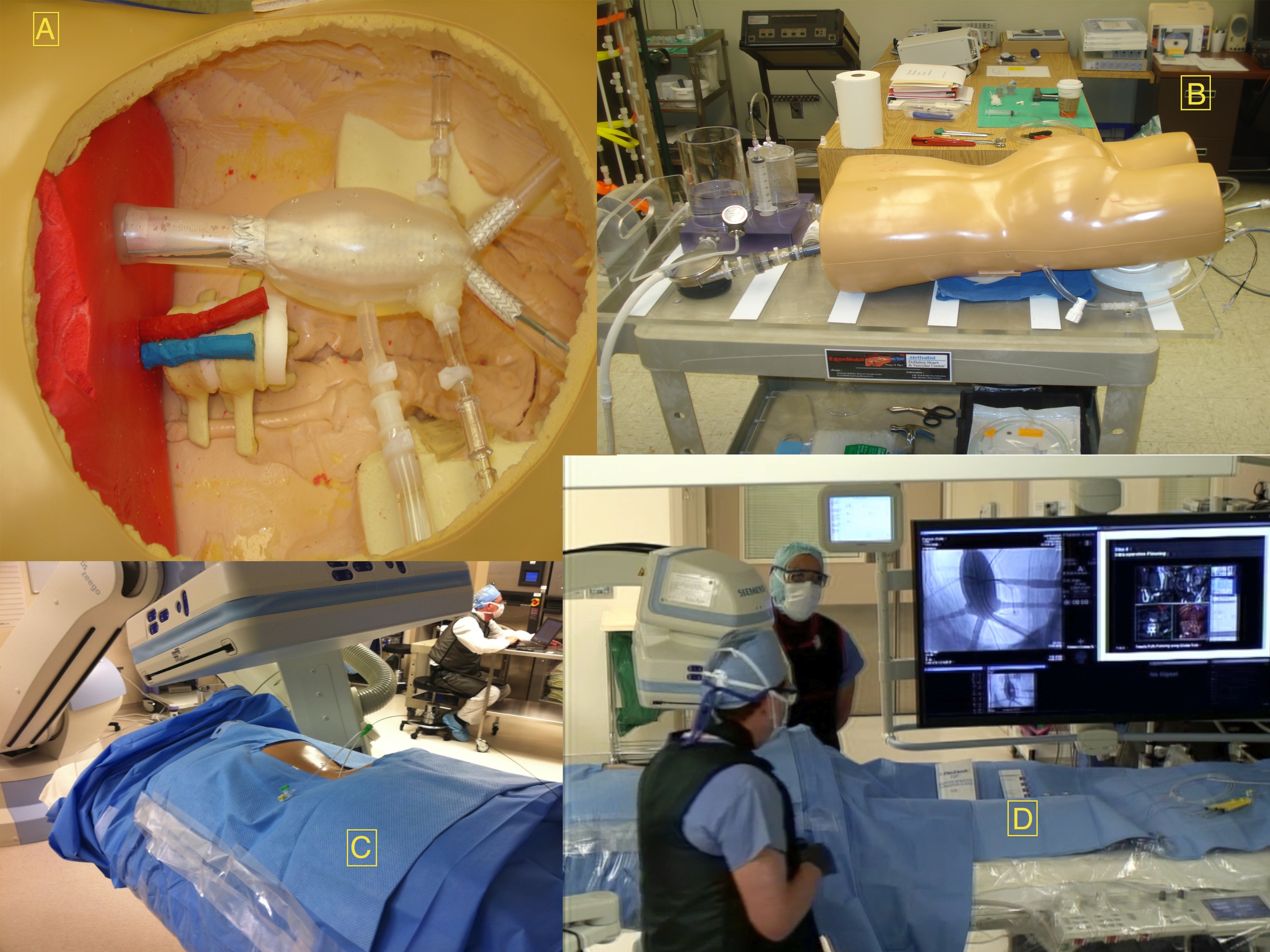
Methods: We developed a simulator-based educational program, which provided instruction on relevant anatomy and pathology, demonstrated the steps to the procedure including the imaging (3D angioCT reconstruction with iGuide), as well as define and demonstrate pitfalls. The simulator was made from multiple materials including a procedure specific silicone aortic model, a mannequin, and pulsatile flow pump (Image: A) silicone model B) Entire model prone C) Translumbar access with sheath in place D) AngioCT in OR) . An aortic endograft was placed to exclude the aneurysm and the silicone aortic model provided an endoleak. Translumbar access was demonstrated, with needle entry into the aneurysm sac. Participants were asked to complete a questionnaire on their experience with the course and model, rating on a standard Likert 5 point scale.
Results: 21 participants completed the questionnaire and rated the course. Average scores gave faculty knowledge 4.7, teaching strategy 4.6, and teaching effectiveness 4.4. Based on the participants’ evaluations and the ability to demonstrate all steps of the procedure we were able establish face validity of the model.
Conclusions: This demonstrates the ability to create models to teach complex endovascular skills. Although this provides a good model and curriculum it does not allow for performance assessment, as individual attendees were not given the opportunity to test their skills. The next step in this process is to evaluate individual performance of experienced interventionalists to establish construct and content validity. 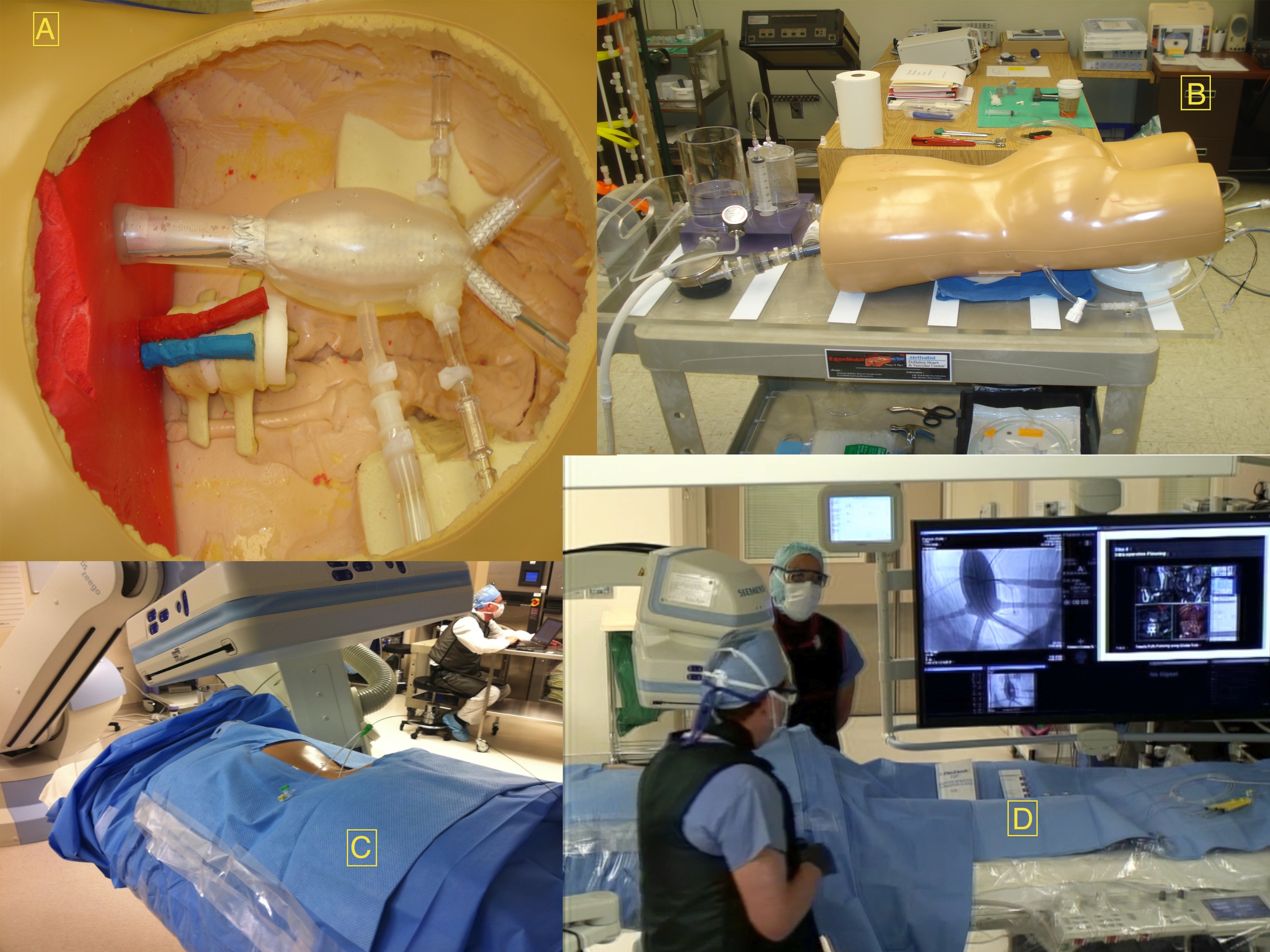
Back to Annual Symposium Program

|