|
Back to Annual Symposium Program
Endovascular Exclusion of a Large External Iliac Vein Aneurysm: A Novel Approach
Mina Todorov, MD, Diego Hernandez, MD.
St. Joseph Mercy Oakland, Pontiac, MI, USA.
OBJECTIVES:
Venous aneurysms are uncommon entities, particularly those involving the iliac veins. Their etiology is often secondary to trauma, and although usually asymptomatic, these aneurysms may lead to complications such as compression, thrombosis, embolization and rupture. Due to their rare occurrence, there has been no consensus as to what constitutes optimal treatment. Historically, these aneurysms have been treated by open techniques with tangential aneurysmectomy and lateral venorrhaphy, or by interposition grafting using other venous or synthetic conduits. We present a case of a large external iliac vein aneurysm successfully treated by endovascular exclusion.
METHODS:
The patient is a 62 year-old male who underwent work-up for a left pelvic mass incidentally discovered during routine urological examination. An MRI confirmed a large saccular external iliac vein aneurysm. As a teenager, he had developed an AV fistula from a traumatic injury to his SFA. He subsequently developed heart failure and the fistula was ligated. For years he had persistent left lower extremity edema previously attributed to a left ankle fracture.
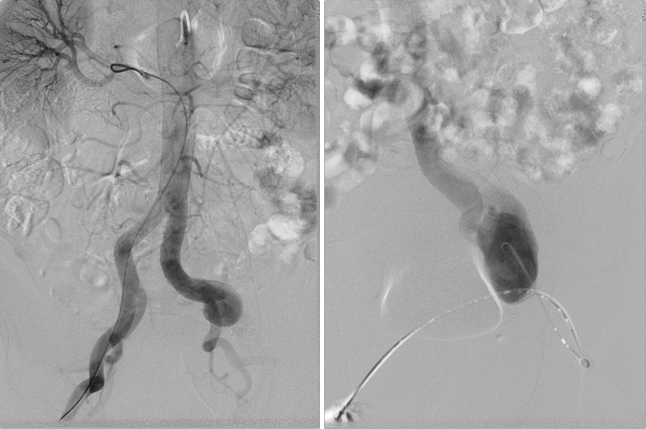
Aorto-iliac angiogram revealed a corkscrew appearance to his dilated left external iliac artery (Figure 1, left image), a sequela of his distal AV fistula. Ascending venogram confirmed a large saccular external iliac vein aneurysm extending just cranial to the common femoral vein, and stenosis of the distal left common iliac vein (Figure 1, right image), likely secondary to compression from the tortuous iliac artery. The aneurysm was excluded by using a 16mm x 18mm x 13.5cm Gore Excluder stent graft. Our access was via cut-down on the mid-femoral vein, and we utilized IVUS to obtain appropriate measurements and ensure adequate positioning.
RESULTS:
Post-deployment venogram confirmed complete aneurysm exclusion and no endoleak. He was discharged home on POD 2 and resumed his daily activities without limitations. He used a compression stocking to control his edema, which resolved quickly. Six month venous Duplex revealed a smaller aneurysm sac and no endoleak.
CONCLUSIONS:
To our knowledge, this is the first reported case of a large external iliac vein aneurysm treated by endovascular exclusion. We have demonstrated the feasibility of this approach, with short-term follow-up that appears satisfactory. 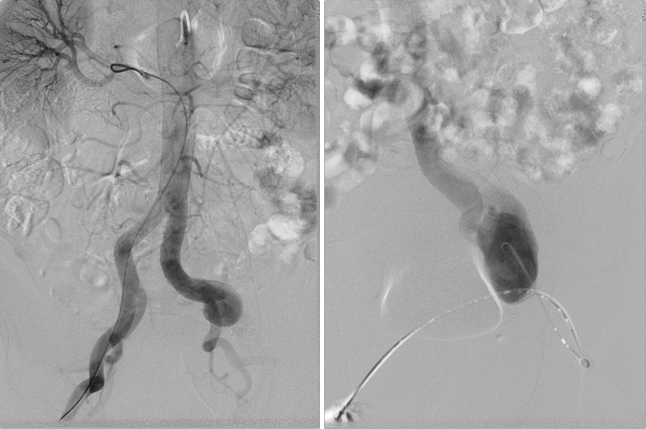
Back to Annual Symposium Program

|