|
|
 |
Back to Annual Meeting Program
Growing Impact Of Restenosis On The Surgical Treatment Of Peripheral Arterial Disease
Douglas W. Jones, MD1, Andres Schanzer, MD2, Yuanyuan Zhao, MS3, Michael S. Conte, MD4, Philip P. Goodney, MD, MS3.
1New York Presbyterian Hospital - Weill-Cornell Medical Center, New York, NY, 2University of Massachusetts Medical School, Worcester, MA, 3Dartmouth Hitchcock Medical Center, Lebanon, NH, 4University of California, San Francisco, San Francisco, CA
Objectives:
Primary peripheral vascular interventions (PVI) and surgical bypass often suffer from restenosis, and secondary procedures performed following restenosis may have poorer outcomes. We investigated how commonly lower extremity bypass (LEB) is performed in the setting of a prior PVI or surgical bypass (“secondary LEB”), and how the outcomes of secondary LEB compare to primary LEB.
Methods:
Within the Vascular Surgery Group of New England (VSGNE), we studied 3,504 patients who underwent LEB (2003-2011). We compared utilization, indications, and outcomes between patients who had primary versus secondary LEB. In-hospital outcomes and outcomes at 1-year follow-up were analyzed and inverse propensity weighting was performed to adjust for differences between the two groups. Subgroup analyses were performed to determine the influence of indication (claudication/critical limb ischemia) and prior intervention type (PVI/LEB/both) on outcomes for secondary LEB.
Results:
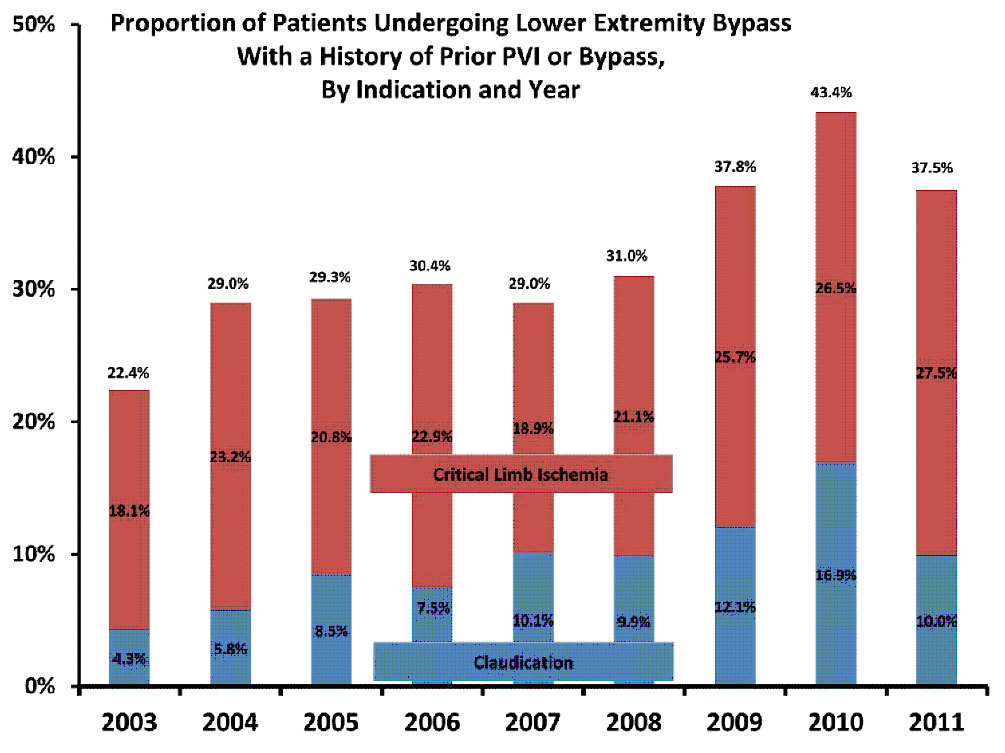
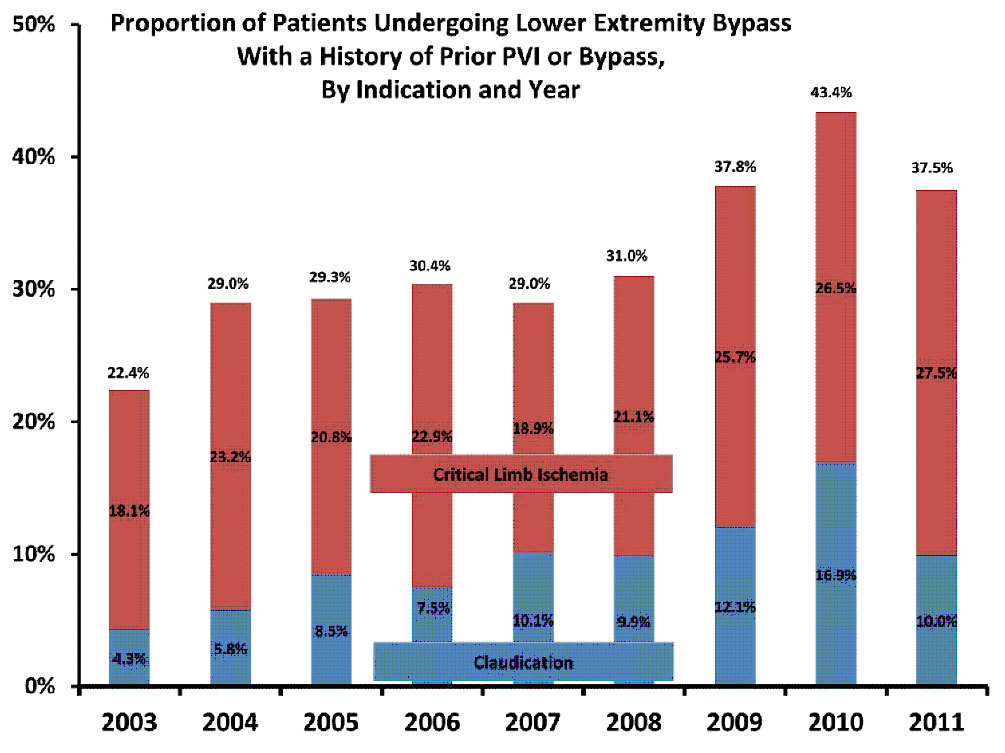
Overall, we studied 2,350 patients undergoing primary LEB, and 1,154 secondary LEB patients who underwent LEB in the setting of a prior PVI (48%), a prior bypass (37%), or both (14%). Of all patients who underwent LEB, the proportion of patients undergoing secondary LEB has doubled over the last nine years (22% in 2003, 38% in 2011, p<0.001). This increase was evident in treatment of patients with CLI (18% to 28% of all LEB, p<0.001) and claudication (4% to 10% of all LEB, p<0.001) (Figure). In crude analyses, rates of in-hospital myocardial infarction (4%), death (2%), or amputation (0.5%) were similar between patients undergoing primary and secondary LEB. However, secondary LEB patients had significantly worse overall freedom from death, reintervention or above-ankle amputation (RAO; 58.9% versus 64.1%, p<0.001), and worse freedom from death or major adverse limb event (MALE; 61.6% versus 67.5%, p<0.001) at 1-year follow-up. These results persisted, even when using inverse propensity weighting to account for differences in patients characteristics. On subgroup analysis, inferior RAO-free survival and MALE-free survival in patients undergoing secondary LEB was independent of the type of prior revascularization (PVI, LEB or both).
Conclusions:
The proportion of patients who undergo LEB as a secondary procedure has increased significantly in recent years, in patients with both claudication and CLI, and their associated outcomes are worse. In an era where many advocate an endovascular first approach to all patients with lower extremity PAD, physicians should consider the first intervention carefully, not only because of the potential immediate implications, but also because of the implications of treatment failure on future events.
Figure:
Back to Annual Meeting Posters

|