|
|
 |
Back to Annual Meeting Program
Increased Risk for Adverse Events following Re-intervention in Patients with Restenosis after prior CEA
Margriet Fokkema, MD1, Gert Jan de Borst, MD PhD2, Brian W. Nolan, MD3, Robert A. Cambria, MD4, Richard J. Powell, MD5, Andrew C. Stanley, MD6, Marc L. Schermerhorn, MD1.
1Beth Israel Deaconess Medical Center, Boston, MA, USA, 2University Medical Center Utrecht, Utrecht, Netherlands, 3Darthmouth-Hitchcock Medical Center, Lebanon, NH, USA, 4Eastern Maine Medical Center, Bangor, ME, USA, 5Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA, 6Fletcher Allen Health Care, Burlington, VT, USA.
OBJECTIVES - Outcomes of patients undergoing re-intervention for restenosis after prior ipsilateral carotid endarterectomy (CEA) in the era of carotid stenting (CAS) are unclear. We assessed perioperative results and durability of CAS and CEA in both symptomatic (sx) and asymptomatic (asx) patients undergoing re-intervention.
METHODS - Patients undergoing CAS and CEA were identified in the Vascular Study Group of New England (VSGNE) between January, 2003, and November, 2011. Demographics, preoperative risk factors, 30-day outcome (stroke/death), cranial nerve injury and restenosis≥50% at follow-up were compared across primary procedures and re-interventions (CAS vs. CEA). Fisher’s Exact test or χ2 test were used to analyze significance differences (P-value <.05) between the different groups.
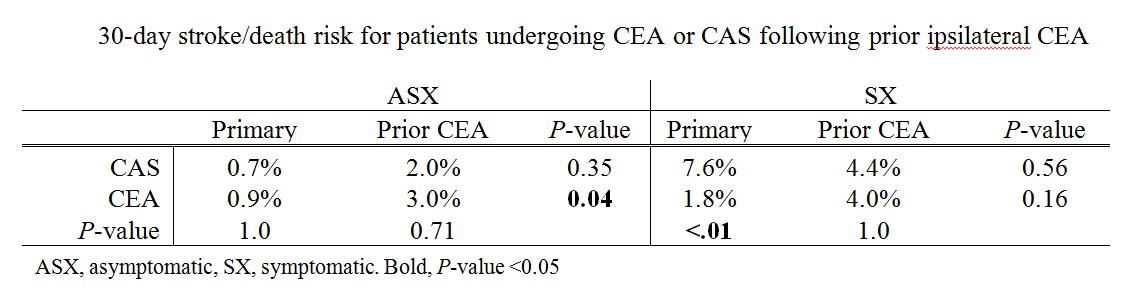
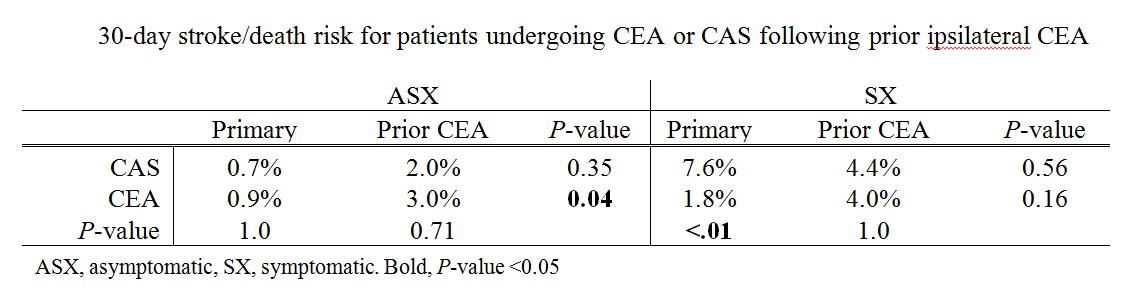
RESULTS - Out of a total of 9357 CEA procedures (33% sx), 212 patients (2.3%) underwent redo-CEA (36% sx). Of 663 CAS procedures (34% sx), 220 patients (33%) underwent CAS after prior ipsilateral CEA (31% sx). Demographics of patients undergoing CAS after prior CEA were comparable to patients undergoing redo-CEA. 40% of CAS patients had at least one medical high-risk factor for CEA. Asymptomatic patients undergoing redo-CEA had a significantly higher stroke/death risk (3.0%) as compared to primary CEA (0.9%), but equivalent to CAS after prior CEA (2.0%). (Table) No difference in perioperative cranial nerve injury was identified between redo-CEA and primary CEA (5.2% vs. 4.7%). Follow-up was available for 56.7% of CAS (median: 254 days) and 68% of CEA patients (median: 370 days). Redo-CEA had higher rates of ≥50%restenosis compared to primary CEA (14.8% vs. 9.8%, P=0.06); there was no significant difference between CAS after prior CEA (17.2%) as compared to redo-CEA (14.8%, P=0.62) and primary CAS (18.6%, P=0.73).
CONCLUSIONS - In the VSGNE, CEA and CAS showed equivalent outcome (30-day stroke/death risk and restenosis) in asx and sx patients treated for restenosis after prior ipsilateral CEA. However, regardless of procedure, the risk of re-intervention was increased as compared to patients undergoing primary CEA.
Back to Annual Meeting Program

|