|
|
 |
Back to Annual Meeting Program
Intramural Hematoma of the Descending Aorta: differences and similarities with acute B Dissection
Jip L. Tolenaar1, MD, Kevin M. Harris2, MD, Gilbert R. Upchurch, Jr.3, MD, Vincenzo Rampoldi1, MD, Arturo Evangelista4, MD, Frans L. Moll5, MD, James B. Froehlich6, MD, Marco di Eusanio7, MD, Kim Eagle6, MD, Santi Trimarchi1, MD.
1Policlinico San Donato IRCCS, Milan, Italy, 2Minneapolis, Minneapolis, MN, USA, 3University of Virginia, Charlottesville, VA, USA, 4Universitari Vall d'Hebron, Barcelona, Spain, 5University of Utrecht, Utrecht, Netherlands, 6University of Michigan, Ann Arbor, MI, USA, 7University of Bologna, Bologna, Italy.
Introduction
Aortic intramural hematoma type B (IMHB) is a relatively rare acute aortic syndrome, which presents with symptoms similar to type B aortic dissection (ABAD). Although the natural history of IMHB seems associated with a less malignant course and better results after medical treatment, such observation is not still totally explored. The purpose of this study was to better characterize IMHB, comparing its clinical characteristics, in-hospital and long-term outcome with patients presenting with classic ABAD.
Methods
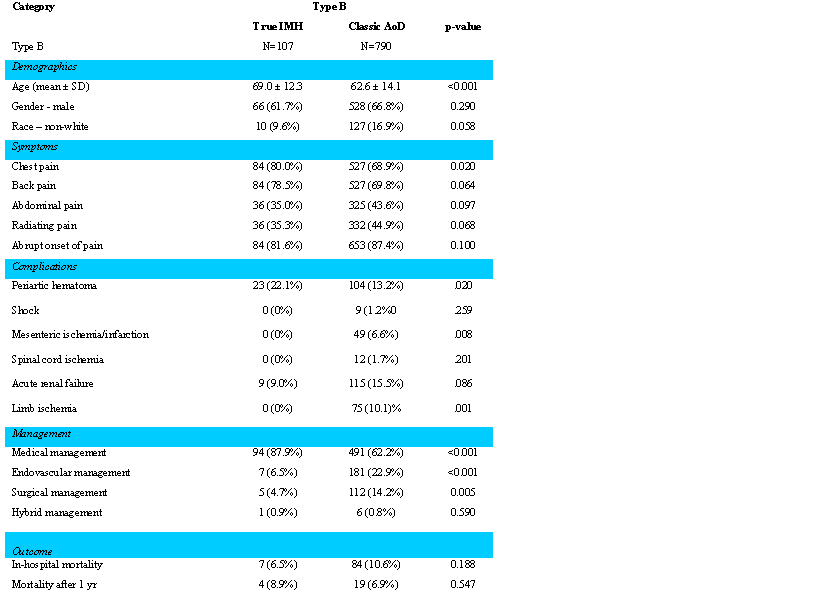
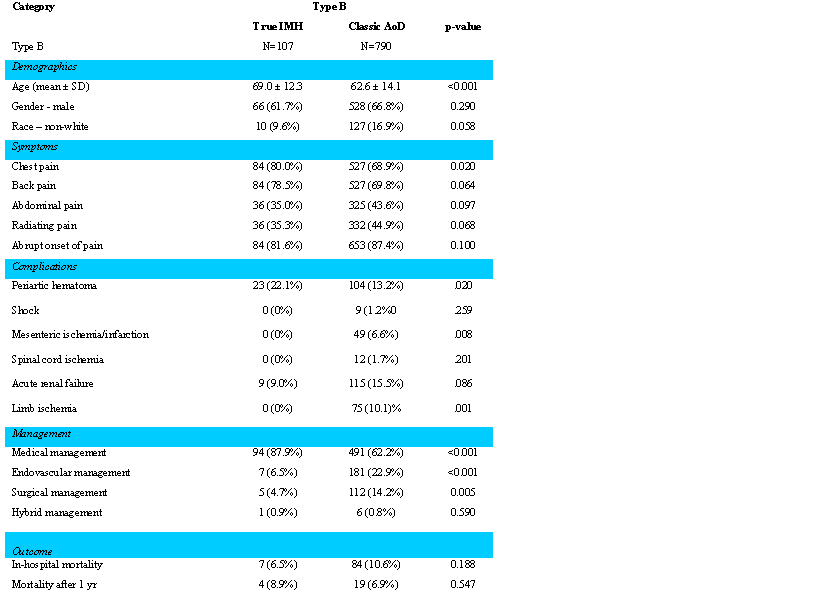
We analyzed 107 IMHB and 790 ABAD patients enrolled in the International Registry of Acute Aortic Dissection (IRAD) between 1996 and 2012. We investigated the differences in presentation, diagnostic, therapy and outcome between these two cohorts.
Results
IMH patients presented at an older age (69.0 vs. 62.6; p < .001) and predominantly in males (61.7%). These patients presented more frequently with chest pain (80.0% vs. 68.9%; p = .020) and periaortic hematoma (22.1% vs. 13.2%; p = .020). IMHB patients were more often treated medically (87.9%) compared to the ABAD patients (62.2%; p < .001), while endovascular or open surgical management, usually reserved for complicated patients were more adopted in ABAD (respectively: endovascular 22.9% vs 6.5%; p= <0.001; open surgical 112 (14.2%) vs 5 (4.7%); p=0.005) Overall in-hospital mortality was 10.1% (89 patients; IMHB 6.5% vs ABAD 10.6%; p = .118) of which 6 IMHB died during medical treatment, two due to aortic rupture. During follow-up, in IMHB patients mortality was 8.9% and no adverse events were observed.
Conclusion
Intramural hematoma of the descending aorta is a serious but rare disease with a relative stable although unpredictable course. Our study confirms that its course is slightly favorable than classic ABAD in the acute setting. In the absence of suitable predictors for high-risk patients, a complication-specific approach should be adopted. Medical treatment combined with adequate follow-up should be administered in all patients, reserving endovascular or surgical intervention for complicated patients.
Back to Annual Meeting Program

|