|
|
 |
Back to Annual Meeting Program
Functional Outcome and Mortality after Open and Endovascular Secondary Intervention for Thoracic Endovascular Aortic Repair
Salvatore T. Scali, M.D., Khayree Butler, M.D., Adam W. Beck, M.D., Robert J. Feezor, M.D., Peter R. Nelson, M.D.,M.P.H., Scott A. Berceli, M.D.,Ph.D., Thomas S. Huber, M.D.,Ph.D., Catherine K. Chang, M.D..
University of Florida-Gainesville, Gainesville, FL, USA.
Objective: Results of thoracic endovascular aortic repair(TEVAR) have demonstrated improved morbidity and short-term mortality compared to open repair; however, concerns about long-term durability remain. The purpose of this analysis was to evaluate incidence of secondary interventions(SI) after TEVAR and determine functional outcomes and survival.
Methods: Retrospective review was completed of all TEVAR patients
from 2004-2011. Patients with SI were further analyzed. A validated questionnaire(ECOG score) was used to assess ability to perform activities of daily living. Kaplan Meier analysis was used to estimate survival.
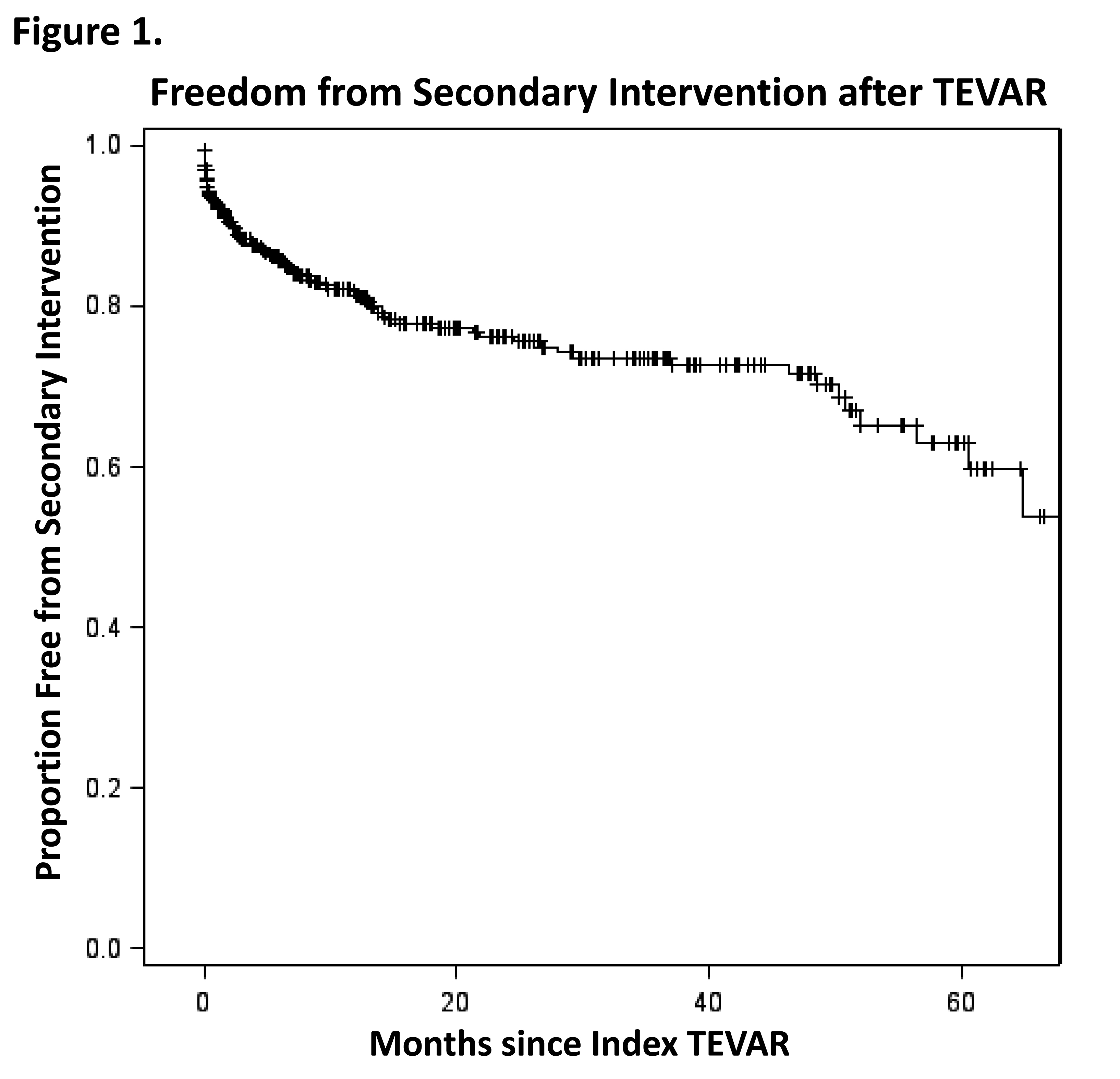
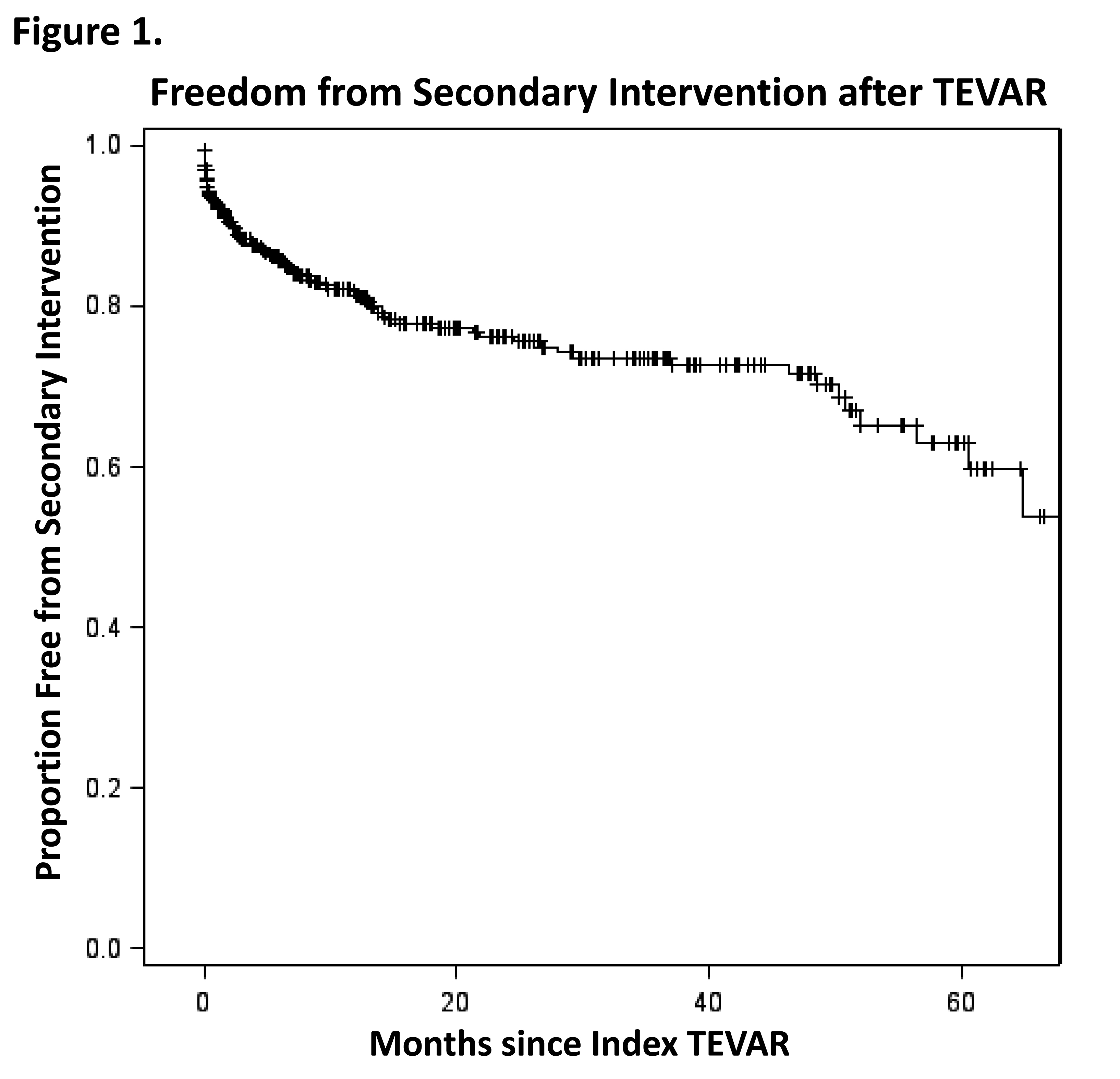
Results: Of 587 patients, 78(13%) required SI at median time of 4.7months(mean±SD:11.5±16.5,Figure 1). Seventeen(22%) underwent multiple SI. Forty(6.8%) initially underwent endovascular revision, with 6(15%) requiring subsequent open reintervention. Thirty-eight(6.5%) initially had open revision, with 6(16%) requiring subsequent endovascular remediation. Median time to endovascular SI was 7.6 months(16.0±18.8), which was significantly longer than time to open SI(1.9 months;6.9±12.3;P=0.01). SI incidence differed significantly amongst various indications(P=.005):acute dissection(24.7%), chronic dissection(16.5%), degenerative aneurysm(14.1%), traumatic transection(8.3%), penetrating ulcer(1.5%), and other miscellaneous(thoracoabdominal aneurysms, mycotic aneurysms, pseudoaneurysms:17.8%). Most common indications for SI after acute/chronic dissection were persistent false lumen perfusion and/or proximal/distal extension of disease whereas for degenerative aneurysms, SI was performed primarily to treat type I/III endoleaks. SI patients had more comorbidities(P<0.0001) and greater number of postoperative complications following the index TEVAR(P<0.0001) compared to those without SI. No survival difference was noted between the groups(SI vs. No SI;P=0.93,Figure 2). At median follow-up of 20.4months(range 6-52), functional status was significantly better among patients first treated with endovascular SI compared to open revision(ECOG scale:1.7±2.1 vs. 2.7±2.1,P=.04).
Conclusion: SI after TEVAR is common, particularly amongst patients
treated for acute dissection, which underscores the need for vigilant
surveillance. Although significant functional impairment is noted after SI for TEVAR, patients can be successfully treated with open and endovascular techniques with no significant increase in long term mortality.
Back to Annual Meeting Program

|