|
|
 |
Back to Annual Meeting Program
Outcomes of lower extremity bypass performed for acute limb ischemia
Donald T. Baril, MD1, Virendra I. Patel, MD2, Dejah R. Judelson, MD1, Philip P. Goodney, MD3, James T. McPhee, MD4, Scott G. Prushik, MD5, Nathanael Hevelone, MPH6, Jack L. Cronenwett, MD3, Andres Schanzer, MD1.
1University of Massachusetts Medical Center, Worcester, MA, USA, 2Massachusetts General Hospital, Boston, MA, USA, 3Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA, 4Boston Medical Center, Boston, MA, USA, 5St. Elizabeth's Medical Center, Boston, MA, USA, 6Harvard School of Public Health, Boston, MA, USA.
OBJECTIVES:
Acute limb ischemia (ALI) remains one of the most challenging emergencies in vascular surgery. Historically, outcomes following interventions for ALI have been associated with high rates of morbidity and mortality. The purpose of this study was to determine contemporary outcomes following lower extremity bypass(LEB) performed for ALI.
METHODS:
All patients undergoing infrainguinal LEB between 2003 and 2011 within hospitals comprising the Vascular Study Group of New England(VSGNE) were identified. Patients were stratified according to whether or not the indication for LEB was ALI. Primary endpoints included bypass graft occlusion, major amputation, and mortality at one year post-operatively as determined by Kaplan-Meier life-table analyses. Multivariable cox proportional hazards models were constructed to evaluate independent predictors of mortality and major amputation at one year.
RESULTS:
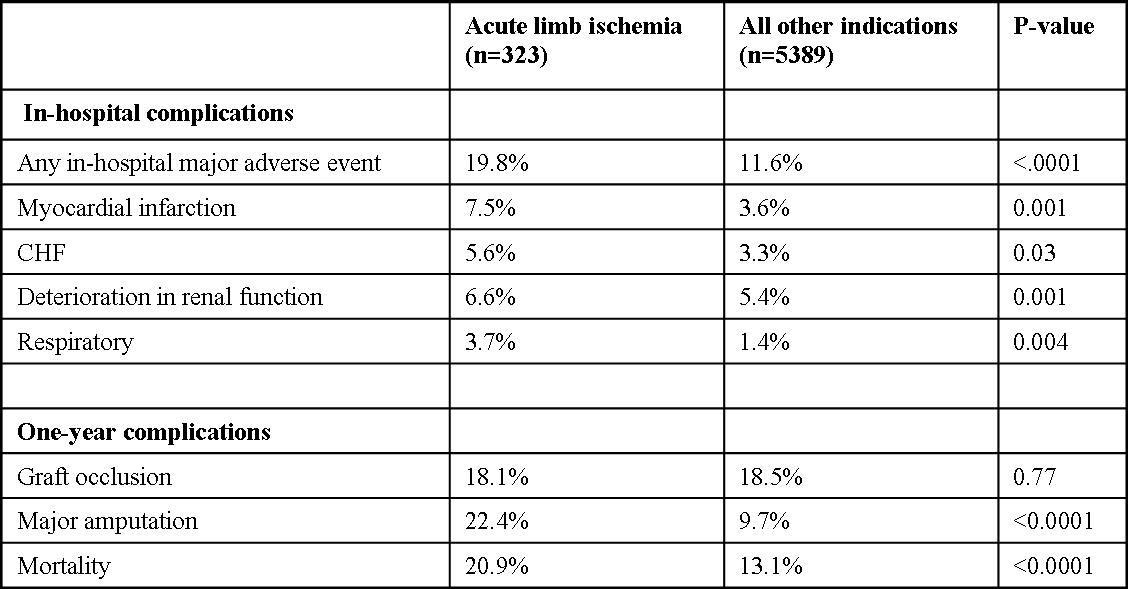
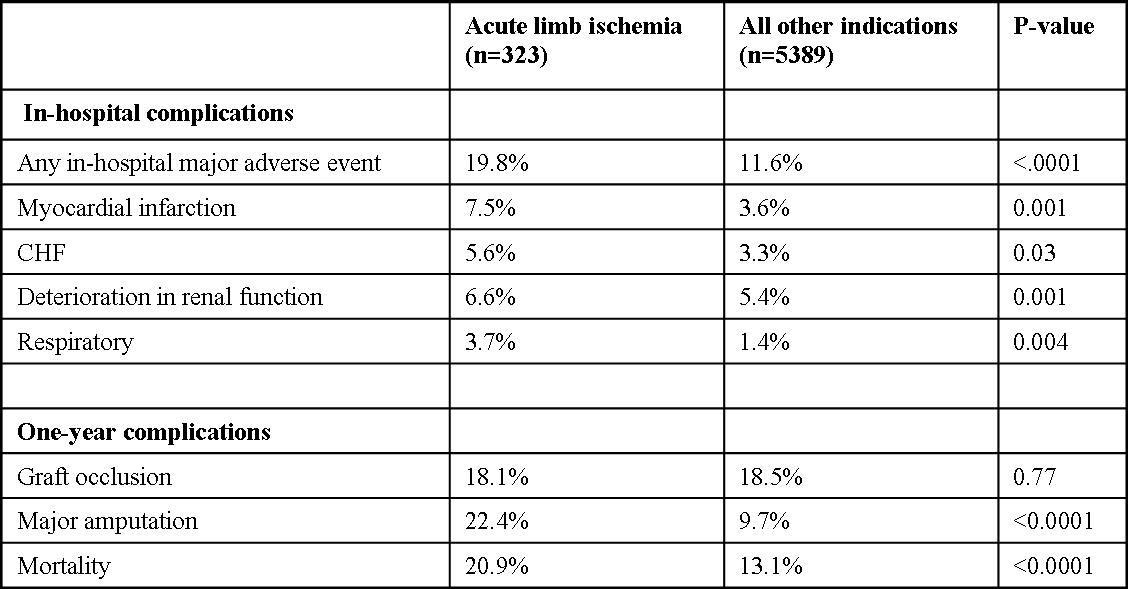
Of 5712 LEB procedures, 323 (5.7%) were performed for ALI. Patients undergoing LEB for ALI were similar in age(66 vs. 67,p=0.084) and gender(68% male vs. 69% male,p=0.617), but were less likely to be on aspirin(63% vs. 75%, p<.0001) or a statin(55% vs. 68%,p<.0001). Patients with ALI were more likely to be current smokers(49% vs. 39%,p<.0001), to have had a prior ipsilateral bypass(33% vs. 24%,p=0.004) or a prior ipsilateral percutaneous intervention(41% vs. 29%, p=0.001). Bypasses performed for ALI were longer in duration(270 vs. 244 minutes,p<.0001), had greater blood loss(363mL vs. 272mL,p<.0001), and more commonly utilized prosthetic conduits(41% vs. 33%,p=0.003). ALI patients experienced increased in-hospital major adverse events including MI, CHF, deterioration in renal function, and respiratory complications(Table 1). Patients who underwent LEB for ALI had no difference in rates of graft occlusion, but did have significantly higher rates of limb loss and mortality at one year(Table 1). On multivariate analysis, ALI was an independent predictor of both major amputation(HR 2.16,CI 1.38-3.40,p=0.001) and mortality(HR 1.41,CI 1.09-1.83,p=0.009) at one year.
CONCLUSIONS:
Patients who present with ALI represent a less medically-optimized subgroup within the population of patients undergoing LEB. These patients may be expected to have more complex operations followed by increased rates of perioperative adverse events. Additionally, despite equivalent graft patency rates, patients undergoing LEB for ALI have significantly higher rates of amputation and mortality at one year.
Back to Annual Meeting Program

|