|
Back to Annual Meeting Program
Transarterial Treatment of Congenital Renal Arteriovenous Fistulas
Naiem Nassiri, M.D., Hirra Ali, M.D., Alfio Carroccio, M.D., Robert J. Rosen, M.D.
Lenox Hill Heart & Vascular Institute of New York, New York, NY, USA.
OBJECTIVE: Congenital Renal Arteriovenous Fistulas (CRAVF) represent a distinct and often misdiagnosed clinical entity with characteristic hemodynamic and angiographic features. Treatment is warranted given potential for growth with renal and hemodynamic compromise. We report our experience with a series of treated symptomatic CRAVFs.
METHODS: Over a 10-year period, patients treated for symptomatic CRAVFs (no history of predisposing renal pathology, instrumentation, neoplasm, or trauma) were retrospectively investigated for clinical presentation, radiographic features, treatment outcomes, and complications. A technically successful treatment included successful delivery of embolic agent with complete obliteration of fistula. Clinical success included resolution of symptoms and freedom from recurrence and reintervention. Renal parenchymal loss as demonstrated by post- embolization angiography was categorized as [0%], [<25%], [25-50%], or [>50%].
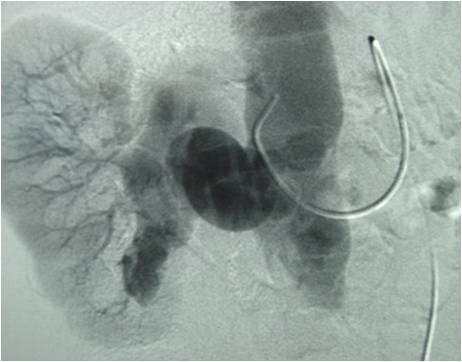
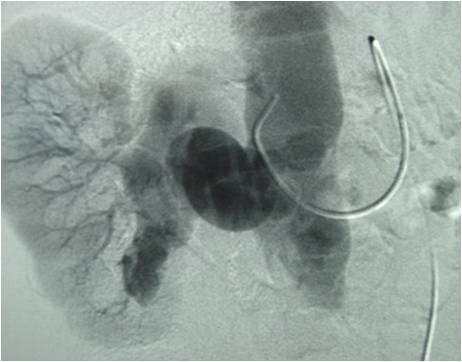
RESULTS: Twenty-five patients were referred with a presumptive diagnosis of intraparenchymal renal artery aneurysm. Of these, 10 had true intrarenal aneurysms, 3 had angiomyolipomas, and 12 had CRAVFs (mean age 54; range 29-71; 8 women). Presenting symptoms included gross hematuria (8), refractory hypertension (diastolic blood pressure ≥ 90 mmHg despite ≥ 3 medications) (6), flank pain (8), high-output state (HOS) (featuring tachycardia and jugular venous distention [JVD]) (3), and flank bruit (1). Defining angiographic features included a high-flow arteriovenous fistula fed by a single, enlarged intrarenal branch shunting into a dilated vein, occasionally featuring a calcified rim (4 patients). All patients underwent transarterial embolization with coils (5), coils and n-butylcyanoacrylate (n-BCA) (3), detachable balloons (2), or Amplatzer plugs (2). Technical success was 100%. Hematuria, tachycardia, JVD, pain, and bruit resolved in all. Hypertension improved in 4 of 6 patients (required 1 medication post-embolization). Complications included a transient, self-limited post-procedural flank discomfort in 9 patients. Parenchymal loss was limited to <25% and occurred in 5 patients. There were no recurrences or reinterventions at a mean follow-up of 55 months (range 5-96). There was 1 death at 8 years follow-up from intercurrent coronary disease in a patient without HOS.
CONCLUSIONS: CRAVF is a rare and likely under-diagnosed clinical entity. With greater awareness and accurate diagnosis, effective and durable transarterial treatment can be safely performed.
Back to Annual Meeting Program

|