|
|
 |
Back to Annual Meeting Program
High Fidelity Virtual Reality Surgical Crisis Simulation: Endovascular Repair of Ruptured Abdominal Aortic Aneurysm
Nung Rudarakanchana, MD, Isabelle Van Herzeele, MD, Colin Bicknell, MD, Celia Riga, MD, Alexander Rolls, MD, Mohamad Hamady, MD, Nicholas Cheshire, MD.
Imperial College, London, London, United Kingdom.
OBJECTIVES:
Endovascular repair of ruptured abdominal aortic aneurysm (rEVAR) may have advantages over open surgery but successful performance of this complex emergency procedure requires trained specialists and multidisciplinary teams. Simulation training may be the key to bridging the gap between declining real-world experience and improving patient outcomes. In this study we report endovascular experts’ evaluation of fully immersive high fidelity virtual reality surgical crisis simulation of rEVAR.
METHODS:
A simulated hybrid operating suite (ORCAMP, Orzone, Sweden), consisting of a fully mobile C-arm and control panel, was integrated with two high fidelity endovascular simulators (VIST-C, Mentice, Sweden) and a ECG simulator (ref), enabling dynamic physiological patient representation.
Six teams, including endovascular specialists, nurses and technicians, were briefed on a standardized scenario and instructed to perform a rEVAR. Mock team members (including anaesthestists, operating department technicians and simulation experts) role-played to provide prompts and further crisis stressors, such as cardiac arrest of the patient, according to team performance against a standardized case timeline.
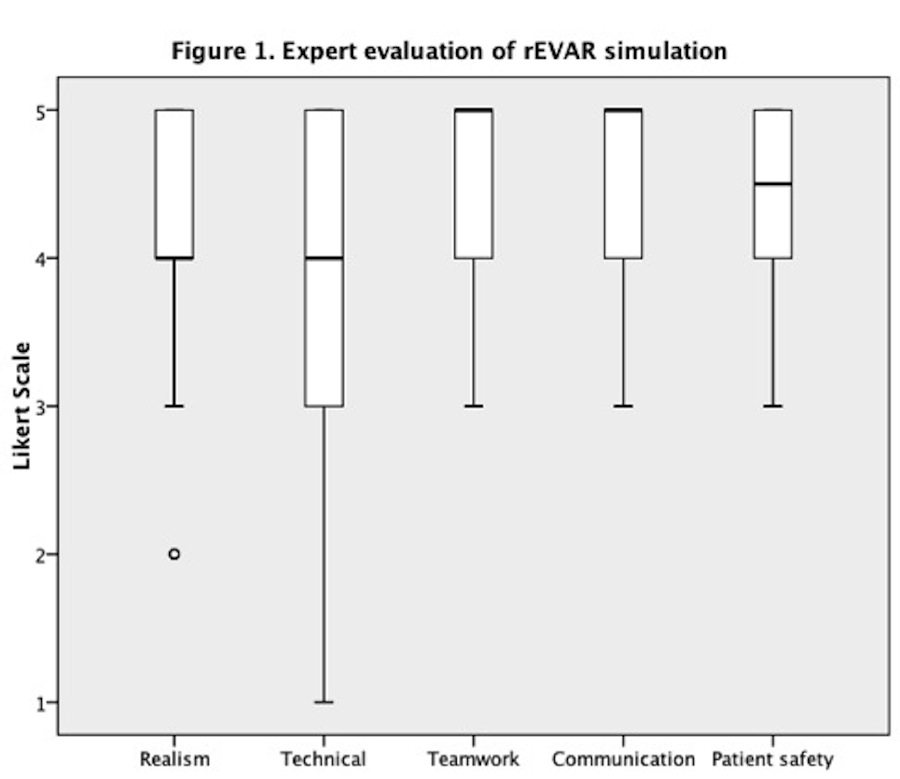
All endovascular specialists (N=6) completed post-procedure questionnaires evaluating realism of the simulated environment and potential for use in training of technical and human factor skills (Likert scale, 1-not at all to 5-very much).
RESULTS:
(Figure 1)
Realism of the simulated angiosuite was scored highly by all endovascular specialists (median 4/5, interquartile range 4-5). Experts found the immersive environment useful for acquiring technical skills (4/5, 2.5-5) and particularly suited to enhancing teamwork (5/5, 4-5) and communication (5/5, 4-5). Moreover, participants believed that the construct had potential to improve patient safety (4.5/5, 3.75-5).
CONCLUSIONS:
Using current technology, fully immersive high fidelity virtual reality simulation of surgical crisis scenarios, such as rEVAR, can be successfully performed. Questionnaire responses appear to validate this specific model in terms of realism and potential use to acquire technical and human factor skills. Capability to improve teamwork and communication skills is particularly important, given that most intraoperative adverse events arise from failures in human factors skills. By enabling deliberate practice and providing objective feedback, fully immersive high fidelity surgical crisis simulation has the potential to enhance performance, reduce errors during high stakes emergency procedures and improve patient safety. 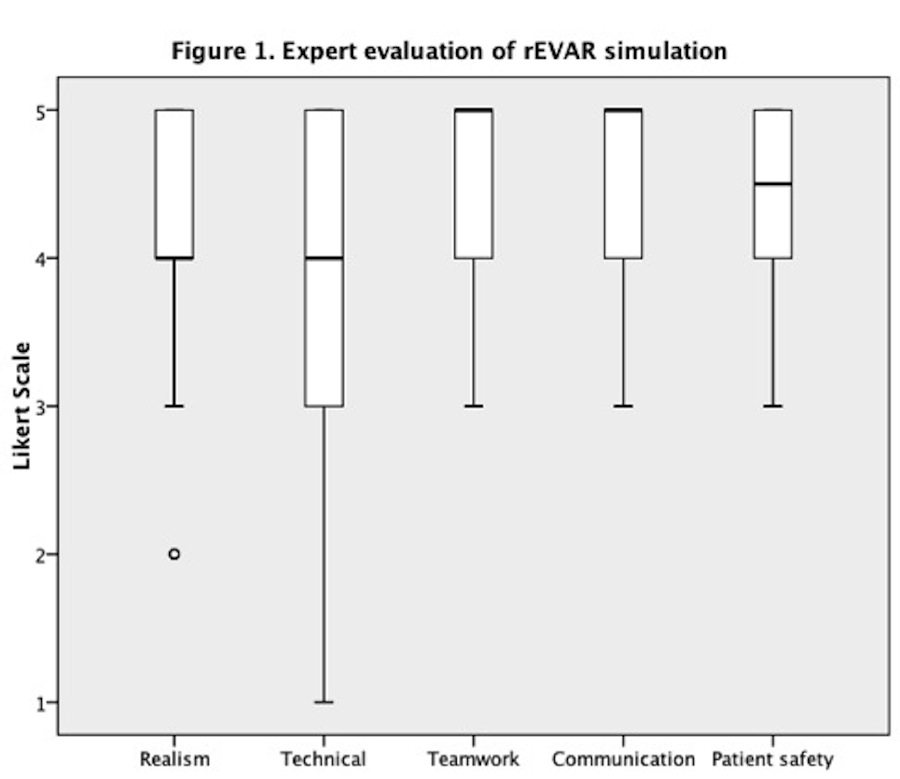
Back to Annual Meeting Program

|