|
|
 |
Back to Annual Meeting Program
Characteristics that Define High Risk in Carotid Endarterectomy from the Vascular Study Group of New England (VSGNE)
Robert Botta1, Felix Schlosser, MD, Ph.D.2, Brian Nolan, MD3, Philip Goodney, MD, MS3, Margriet Fokkema, MD4, Marc Schermerhorn, MD4, Daniel Bertges, MD5, Jeffrey Indes, MD2.
1University of Connecticut School of Medicine, Farmington, CT, USA, 2Yale University School of Medicine, New Haven, CT, USA, 3Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA, 4Beth Israel Deaconess Medical Center, Boston, MA, USA, 5University of Vermont College of Medicine, Burlington, VT, USA.
OBJECTIVES: The SAPPHIRE trial compared carotid endarterectomy (CEA) to carotid artery stenting (CAS) among high risk patients using a model of risk that has not been validated by previous publications. The objective of our study was to determine the accuracy of high risk CAS inclusion criteria, and to define patients at high risk for adverse outcomes after CEA.
METHODS: Prospectively collected data on 3,098 CEA’s between
2003-2011 at 20 VSGNE centers was used for this study. SAPPHIRE general inclusion criteria and primary outcome were used. Risk factors from SAPPHIRE, as well as additional factors described by previous studies (SAPPHIRE +), were compiled for analysis. Factors that were associated with the primary outcome by ANOVA (p<0.10) and not linearly dependent, as determined by a Pearson’s correlation analysis (n=3,098), were further assessed for an independent association by multivariate logistic regression (n=2,839).
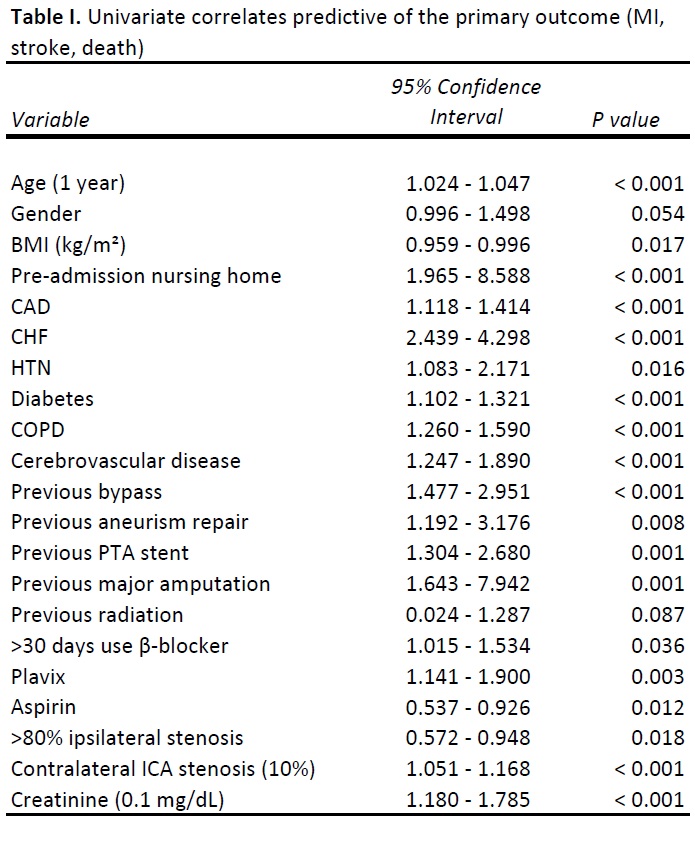
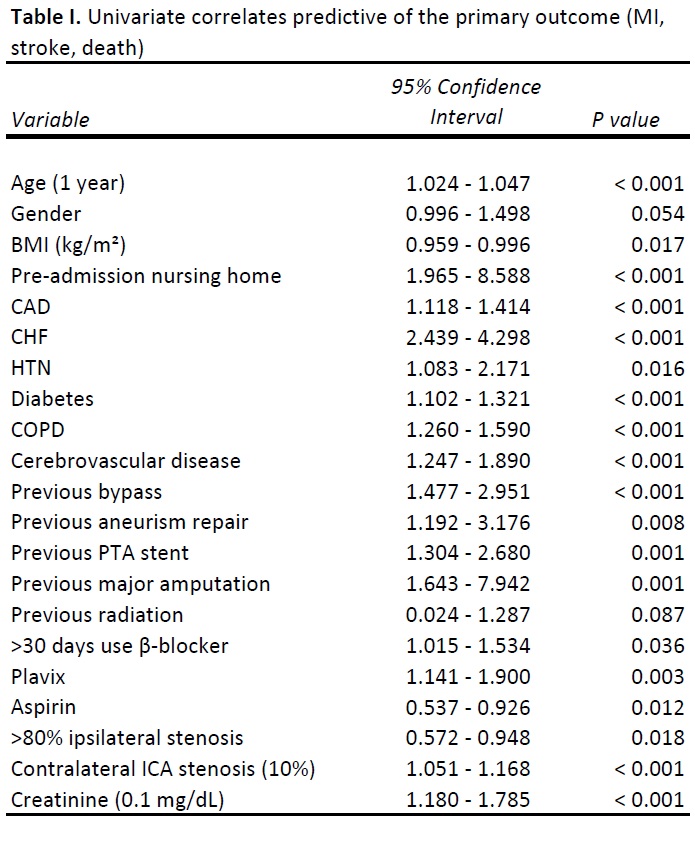
RESULTS: The average age was 69.9±9.5 years, 60% were male, and 45.7% were asymptomatic. The 1-year composite outcome event rate, defined as post-operative MI and 1 year stroke or death, was 14.2%. The SAPPHIRE + factors associated (P<0.10) with the composite outcome by univariate analysis are included in table 1. Multivariate analysis (P<0.05) found the following independently significant risk factors (95% CI; P value): age in years (1.0-1.1; <0.001), pre-admission nursing home (1.2-6.6; 0.020), CHF (1.4-2.8; <0.001), diabetes (1.1-1.3; <0.001), COPD (1.2-1.5; <0.001), any previous cerebrovascular disease (1.1-1.9; 0.003), and contralateral ICA stenosis (1.0-1.2; 0.001). Two of the SAPPHIRE high risk criteria, recurrent stenosis after CEA and previous radiation therapy to the neck, were not, in fact, found to be significantly associated with an adverse outcome.
CONCLUSIONS: SAPPHIRE and other previously reported high risk CAS inclusion criteria have been arbitrarily assigned and do not include factors found to be independently associated with outcome. Further studies, therefore, are required to determine whether stenting is inferior to CEA in high risk endarterectomy using a validated model of risk. Additionally, this pre-operative assessment includes novel criteria that can be used to help stratify CEA patients in a future risk index model.
Back to Annual Meeting Program

|