|
Back to Annual Meeting Program
Variations in Maximum Diameter Measurements of Descending Thoracic Aortic Aneursyms (DTA): Potential Impact on Clinical Practice
Nung Rudarakanchana, Colin Bicknell, Nicholas Cheshire, Nicholas Burfitt, Alexander Chapman, Mohamad Hamady, Janet Powell.
Imperial College, London, London, United Kingdom.
OBJECTIVES:
Current guidelines for intervention for descending thoracic aneurysms (DTA) do not state specific methods for measurement of threshold diameters. Given that the thoracic aorta may be highly angulated, using different planes for measurement may be expected to produce variable results. Optimal measurement methods need to be defined in order to standardise treatment and facilitate trials in this area. In this study we evaluate variation in DTA diameters measured on CT scans and the potential impact of such variation on treatment decisions.
METHODS:
Scans from DTA (N=20, fusiform, diameter range 5-13cm) were assessed, in random order with a defined protocol, by three independent vascular interventional radiologists using CT angiography (Philips-Netherlands). For each scan, calliper measurements of maximum diameter were made on axial images (axial) and perpendicular to aneurysm axis after image-processing (corrected). Repeatability was assessed using Bland-Altman plots, with statistical significance calculated using Student t and Pearson Chi-square tests.
RESULTS:
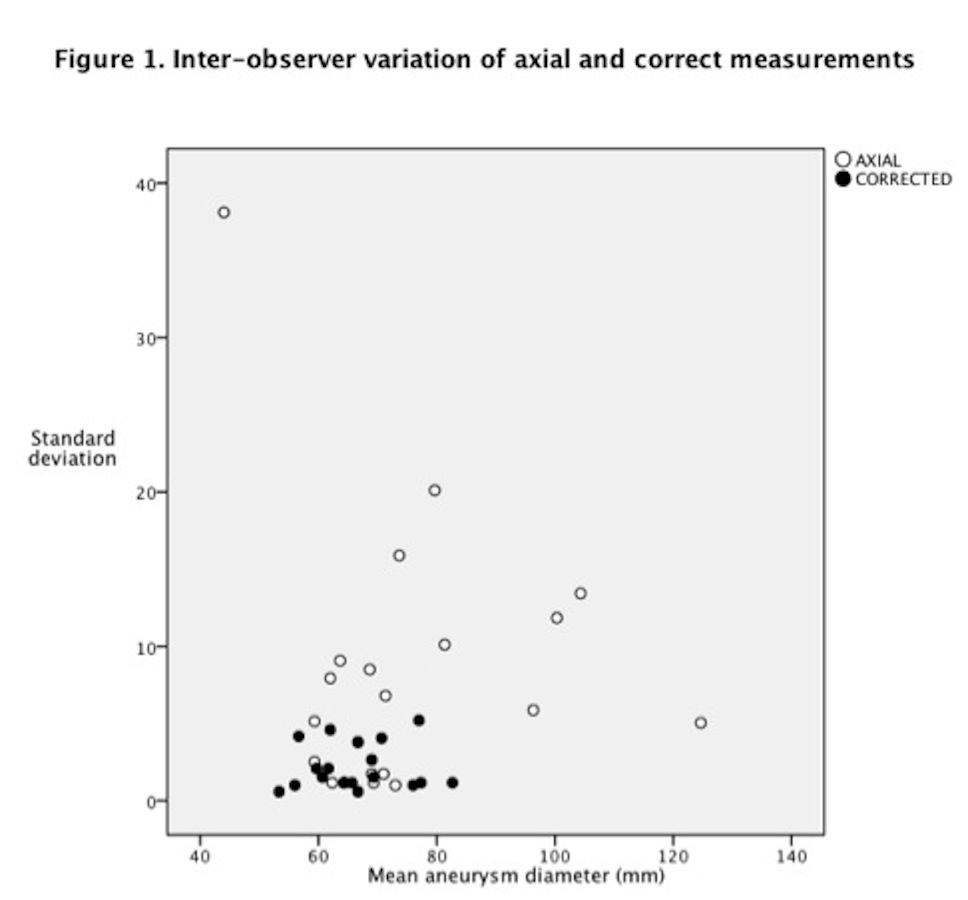
Inter-observer variation was greater on axial than corrected measurements, mean difference 6.8±8.2mm versus 2.8±2.5mm,P<0.01 (Figure 1). This variation increased with aneurysm diameter (50-74mm and 7.5-130mm groups) for axial but not corrected diameters, mean differences respectively 6.1±5.5mm versus 13.8±7.1mm,P<0.01 and 2.8±1.8mm versus 2.5±2.3mm,P=0.99.
Axial measurements were greater than corrected measurements (mean 76.2±18.6mm versus 66.3±7.9mm, P<0.01), and this difference increased with aneurysm diameter (50-74mm,mean difference 3.2±5.2mm versus 75-130mm,27.8±14.6mm, P<0.01).
Using corrected rather than axial measurements could have changed treatment decisions in 4 cases (7%) using the American Heart Association guidelines (threshold 5.5cm) and 18 cases (31%) using Yale guidelines (threshold 6.5cm) (Chi-square=7.17;P<0.01).
CONCLUSIONS:
Corrected diameters were smaller than axial diameters and showed better inter-observer repeatability. Using corrected versus axial measurements would have changed management decisions in up to 31% of cases in this study. Explicit protocol-driven measurement of corrected diameters is crucial to improving management decisions and facilitating randomised controlled trials to establish evidence-based threshold diameters for treatment. 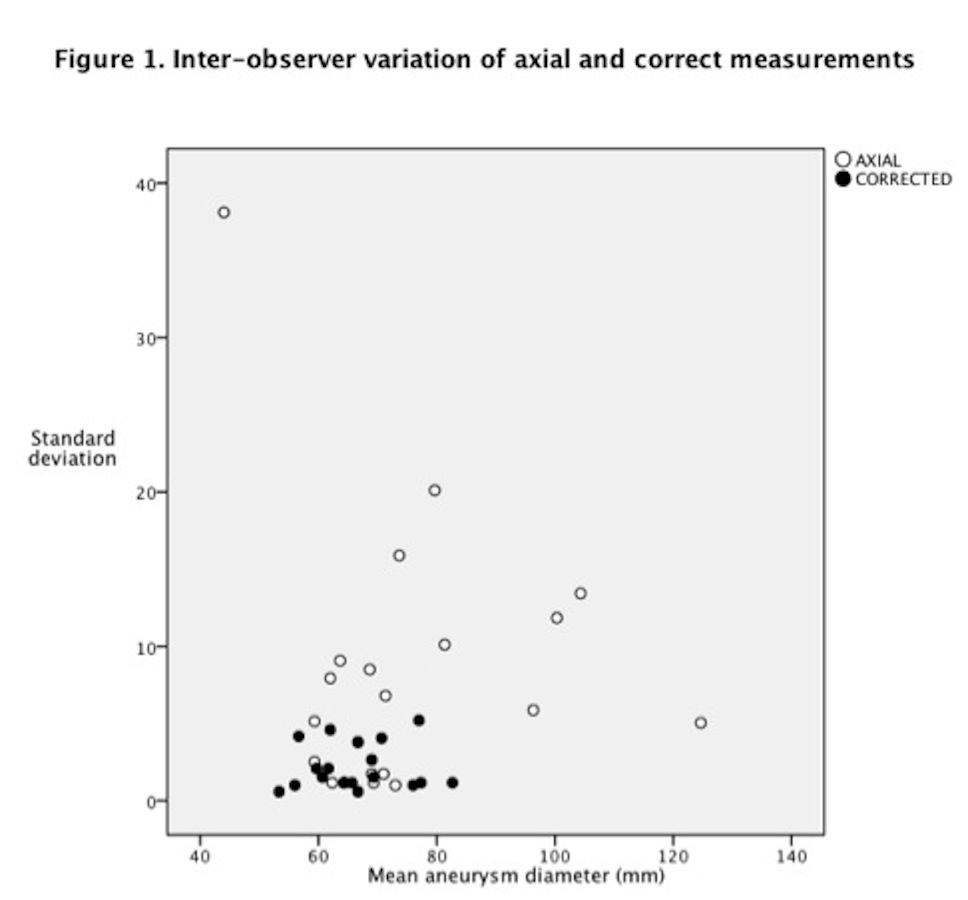
Back to Annual Meeting Program

|