|
|
 |
Back to Annual Meeting Program
Impact of Race and Socioeconomic Status on the Use of Endovascular Repair to Treat Thoracic Aortic Diseases
William F. Johnston, MD, Damien J. LaPar, M.D., Timothy Newhook, M.D., Gilbert R. Upchurch, Jr., M.D., Gorav Ailawadi, M.D..
University of Virginia, Charlottesville, VA, USA.
OBJECTIVES:Descending thoracic aortic diseases may be repaired with either open thoracic aortic repair (OTAR) or thoracic aortic endovascular repair (TEVAR). Since access to care and resource allocation varies based on race and socioeconomic status (SES), we sought to determine the impact of these variables on treatment options for thoracic aortic disease. We hypothesized that racial minorities and lower SES patients have a lower propensity to have their thoracic aortic disease treated with TEVAR.
METHODS: Weighted discharge records for patients who underwent either OTAR and TEVAR between 2005 and 2008 were evaluated using the Nationwide Inpatient Sample. Patient records were stratified by therapeutic intervention (OTAR vs. TEVAR). Differences in baseline risk, race, and SES were compared by univariate analyses. Median household income was assigned according to patient zip code. To account for the effects of multiple variables, hierarchical logistic regression modeling was utilized to estimate the risk-adjusted propensity for the performance of TEVAR as a function of race and SES.
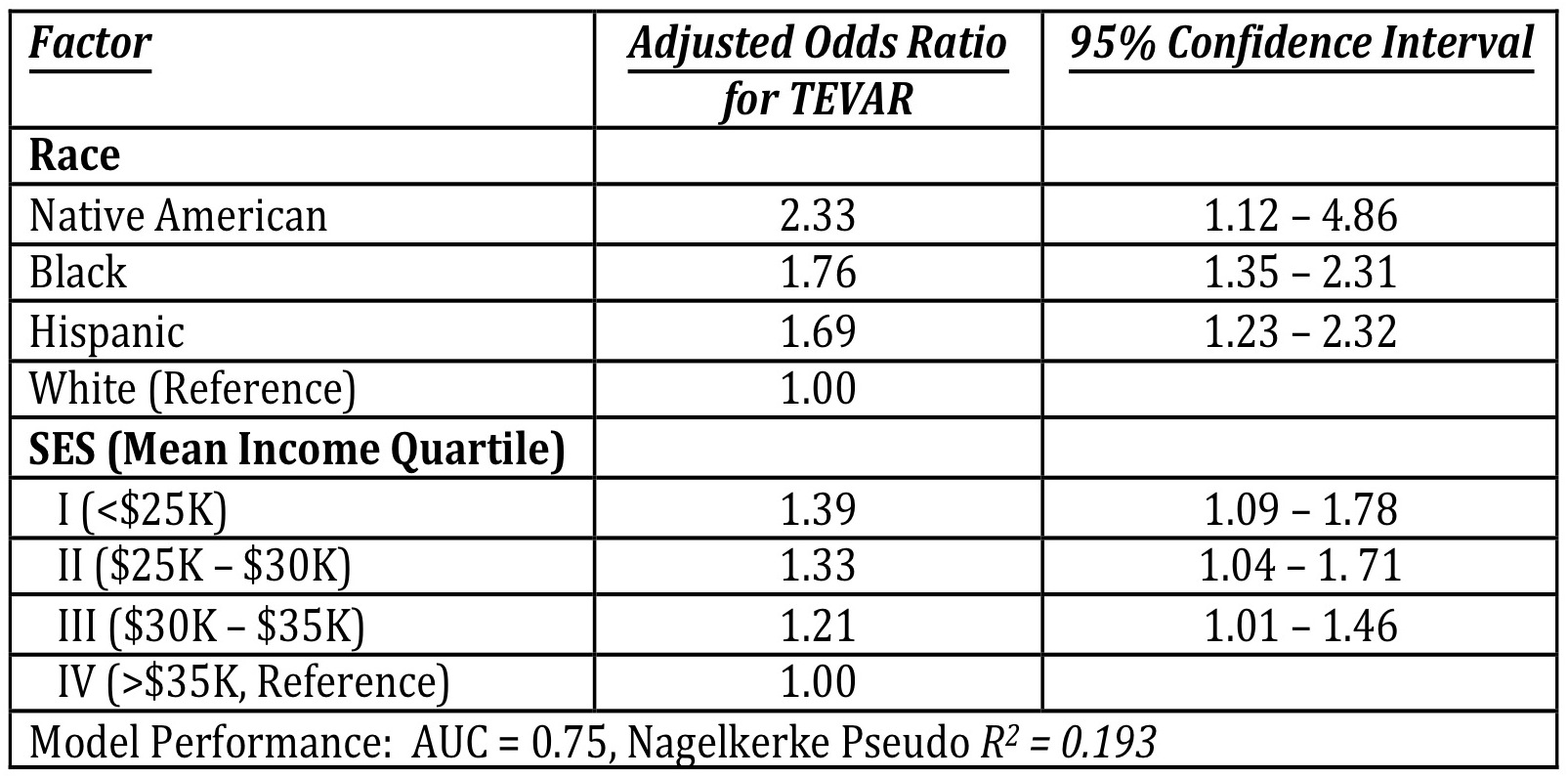
RESULTS: A total of 60,784 OTARs and TEVARs were analyzed, the majority (79.4%) of which were OTAR. Average patient age was 58.7 years, and the majority of patients were male (64.9%). Indications for treatment included: intact thoracic aortic aneurysm (46.1%), thoracic aortic dissection (25.3%), intact thoraco-abdominal aneurysm (6.8%), and ruptured thoracic aortic aneurysm (2.9%). Compared to OTAR, TEVAR was performed in older patients (65.3±0.2 years vs. 57.1±0.1 years) and incurred shorter length of stays (10.5±0.1 days vs. 13.1±0.7 days) and lower total charges ($160,036±1,374 vs. $172,179±705) (p<0.001 for all). Importantly, upon risk adjustment, both race and SES were significantly associated with treatment allocation (Table) with an increased propensity for the performance of TEVAR among Black, Hispanic, and Native-American populations, as well as for those of lower SES.
CONCLUSIONS: Race and socioeconomic status were significantly associated with treatment allocation for thoracic aortic disease within the United States. Contrary to our hypothesis, racial minorities (Black, Hispanic, and Native American) and patients with lower median household incomes have a greater propensity for the performance for TEVAR after accounting for patient comorbid disease, indication for treatment, and payer status. 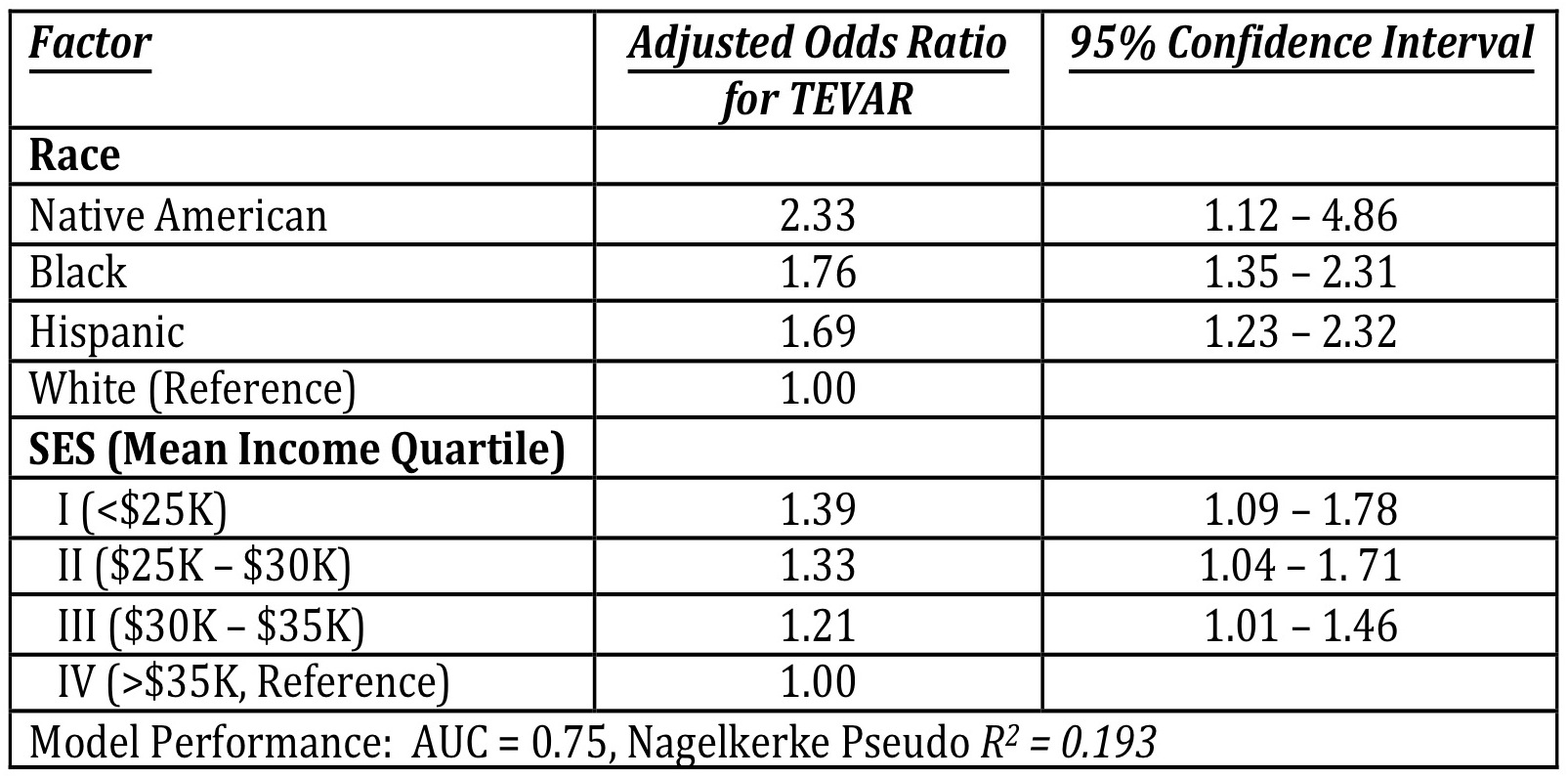
Back to Annual Meeting Program

|