|
Back to Annual Meeting Program
Endovascular Management of Blunt Aortic Injury Is Appropriate Primary Therapy Based on Results Over 17 Years
James A. Davis, Ramyar Gilani, Farhan Zafar, Peter I. Tsai, Mathew J. Wall, Kenneth L. Mattox, Charles A. West.
Baylor College of Medicine, Houston, TX, USA.
Objectives: Traumatic Blunt Aortic Injury (BAI) is a life threatening condition. Surgical treatment options currently include open (OR) and endovascular repair (EV). We reviewed our experience over 17 years to determine appropriate management of patients with BAI.
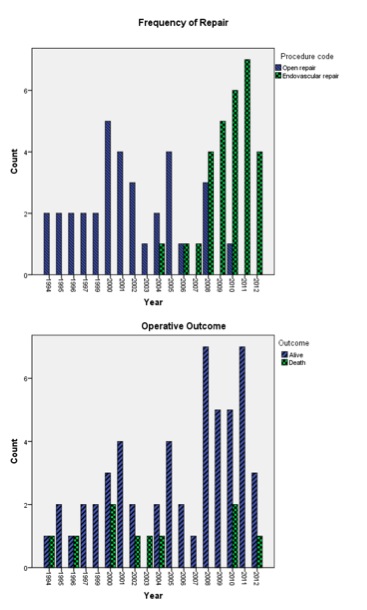
Methods: Retrospective review of a single institution Level I trauma registry was performed from 1994 to 2012 identifying 131 patients having BAI of the descending thoracic aorta. Patients were divided based on non-operative versus operative management which was further divided into OR and EV groups. All groups were analyzed comparing age, injury severity scores (ISS), and mortality. Operative groups were further analyzed comparing intensive care unit (ICU) length of stay (LOS) and hospital LOS as well as procedural, device or access related complications.
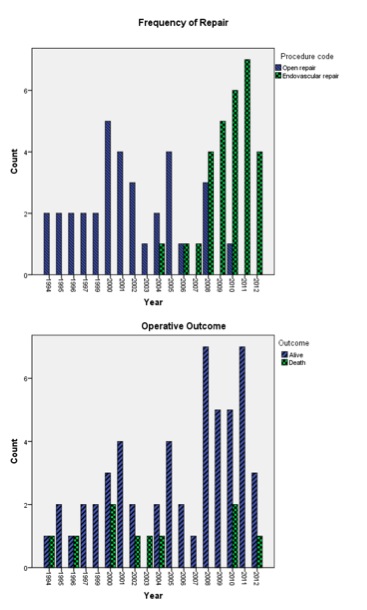
Results: There were 68 patients not receiving surgical intervention with similar age (p=0.98), higher ISS score (50, p<0.001) and mortality (88%, p<0.001) when compared to operative patients. Furthermore, 63 patients underwent operative management via OR (34) or EV (29). Mean age was similar, however, ISS was higher for EV group (36 vs. 30, p=0.02). Mortality trended lower (6.9% vs. 24%, p=0.07) in the EV group. ICU and hospital LOS was similar for operative groups. In the OR group, there were 2 (6%) strokes and 1 (3%) paraplegia. In the EV group, there were no technical failures, strokes, paraplegia or device related complications but 1 (3%) access related complication occurred. Over the last 5 years, 87% of repairs for BAI were EV, however mortality in patients with BAI as a cohort remains unchanged.
Conclusions: BAI continues to be associated with significant mortality regardless of therapy. Despite its use in more severely injured patients, mortality outcomes for patients undergoing TEVAR support its use. Device complications remain infrequent as well as access and procedure related complications. As a result, TEVAR has become the primary mode of therapy for BAI at our institution. Long-term follow-up is still needed to attest durability of repair and if trends in results will continue.
Back to Annual Meeting Program

|