|
Back to Annual Meeting Posters
Analysis of Critical Limb Ischemia Using MRA with Contrast-Enhanced MR Perfusion Scans
Nima Nassiri, John Barakat, Ben Ellingson, Ph.D., John Moriarty, M.D., Peter F. Lawrence, M.D..
University of California, Los Angeles, Los Angeles, CA, USA.
ANALYSIS OF CRITICAL LIMB ISCHEMIA USING MRA WITH CONTRAST-ENHANCED MR PERFUSION SCANS
OBJECTIVES: To determine the perfusion deficit in CLI patients with non-healing wounds of the lower extremity using magnetic resonance angiography (MRA) in combination with 3-dimensional contrast-enhanced MR perfusion.
METHODS: Patients with CLI underwent conventional physiologic lower extremity testing; prior to treatment, patients underwent conventional T1-weighted MRA with 3D reconstruction for anatomy. This study was supplemented with 3D gadolinium-enhanced MR perfusion imaging. All scan were performed on a high field strength 3T Siemens TrioTim MRI scanner. Image acquisition and analysis was performed using Siemens Tissue 4D software, which measures contrast agent concentrations. Perfusion (pharmacokinetic) parameters that were investigated included:
1.
fpv = plasma blood volume fraction
2.
Ktrans = transfer rate reflecting contrast delivery (perfusion) and transport across the vascular endothelium (permeability)
3.
kep = contrast agent efflux/clearance from the extracellular space
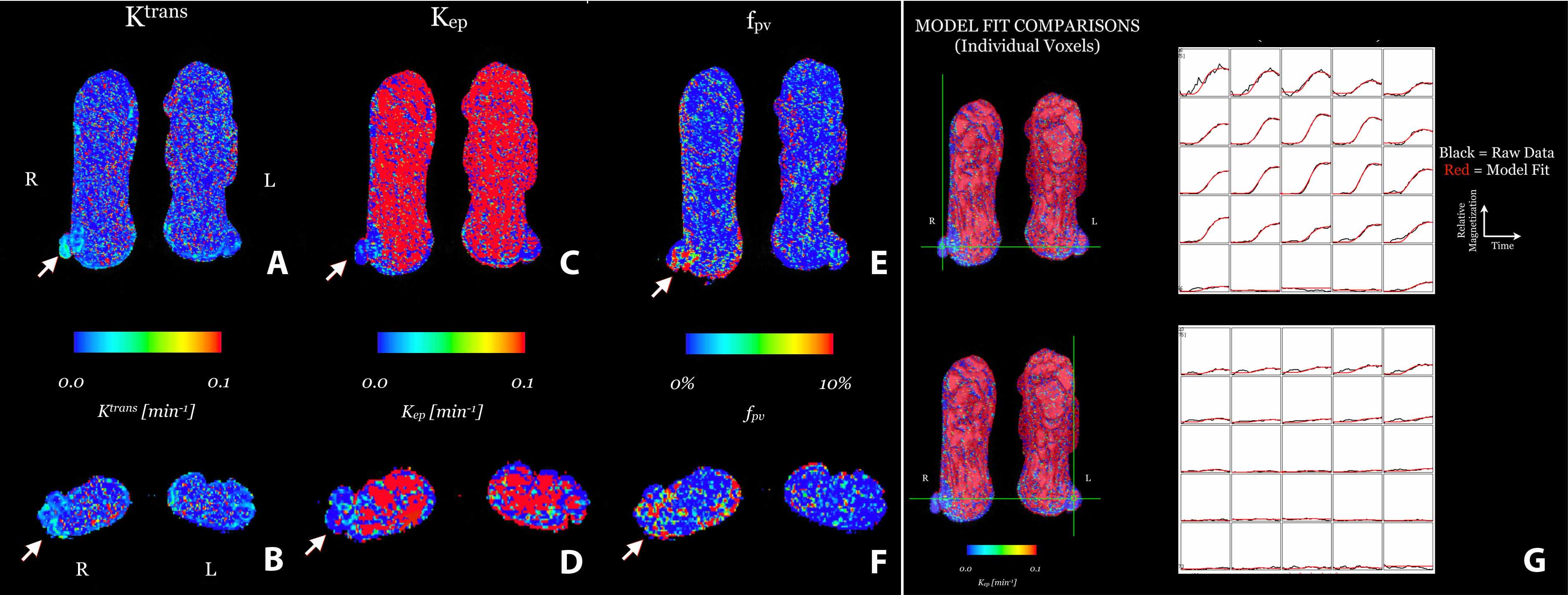
RESULTS: 8 ischemic limbs were evaluated in patients with documented CLI. Average ankle-brachial index (ABI) values = 0.48 (S.D. = 0.23). Qualitative analysis of perfusion revealed focal hypoperfusion at the site of tissue injury (Fig. 1). fpv (unitless, %) increased from control (0.0103±0.0004) to injured (0.03728±0.0011) (p<0.0001). Ktrans (1/min) shows no change between control (0.0143±0.0007) and injured (0.149±0.0006) (p >0.05). Lastly, kep (1/min) decreased from control (2.4514±0.0573) to injured (0.80993±0.0414) (p<0.0001).
Figure 1: 89 year old male patient diagnosed with CLI. Coronal and axial parametric maps of Ktrans (A,B), kep (C,D), and fpv (E,F). Model-fit comparison between limbs (G).
CONCLUSIONS: MRA supplemented with 3D contrast-enhanced MR perfusion allows further assessment of the perfusion deficit in patients with CLI. Preliminary data is promising for using this novel technique for qualitatively and quantitatively evaluating the perfusion deficit in the lower extremities of patients with non-healing wounds. This information may be particularly useful to guide therapeutic intervention when physiological parameters are unreliable, such as elevated ABIs, and to assess the impact of angiosome-related ischemia. 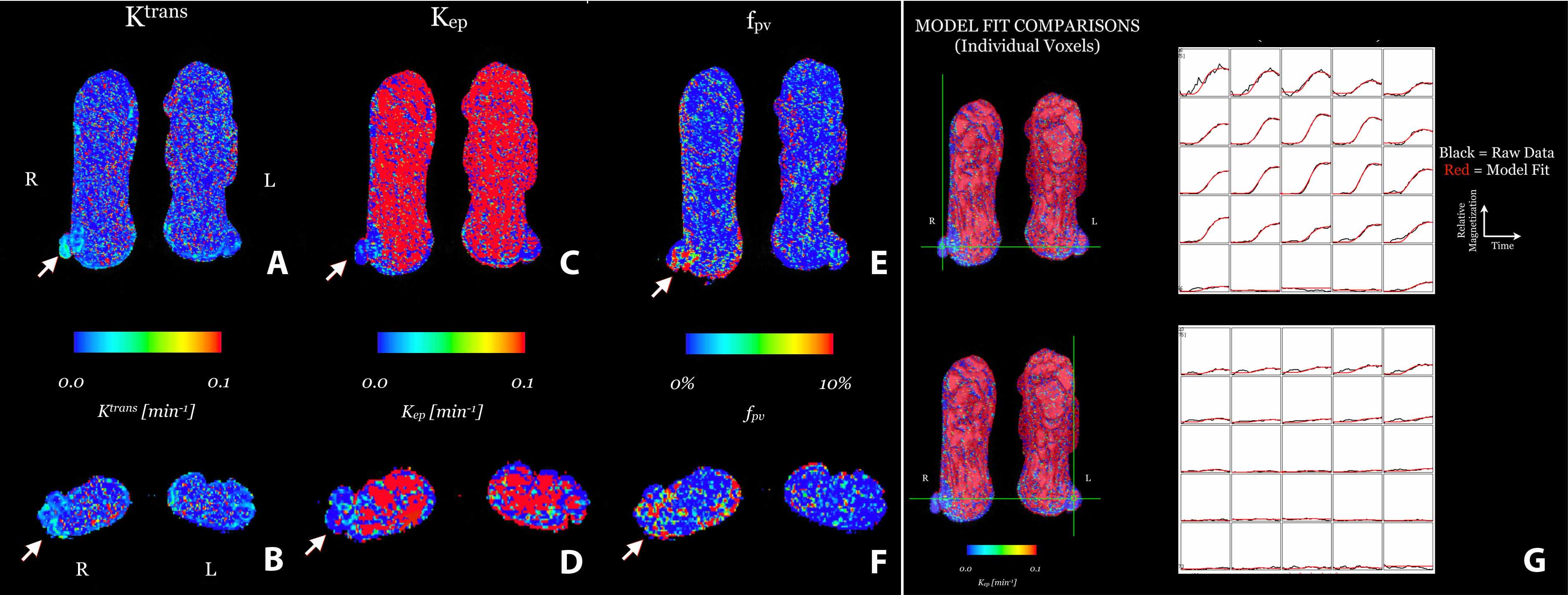
Back to Annual Meeting Posters

|