|
|
 |
Back to Annual Meeting Symposium
Long term Carotid Artery Disease Progression and Related Neurologic Events Following Carotid Endarterectomy
Efthymios D. Avgerinos, MD, Catherine Go, MD, Jennifer Ling, MD, Abdallah Naddaf, MD, Amy L. Steinmetz, Michel S. Makaroun, MD, Rabih A. Chaer, MD.
University of Pittsburgh, Pittsburgh, PA, USA.
OBJECTIVES:
The purpose of the study was to assess predictors of long term disease progression and clinical outcomes following carotid endarterectomy (CEA) in contemporary practice.
METHODS: A consecutive cohort of CEAs between 1/1/2000 - 12/31/2010 was retrospectively analyzed. Endpoints were restenosis ≥50% and ≥70%, contralateral carotid disease progression (50-69%, 70-99% or occlusion) and stroke. Survival analysis and Cox regression models were used to
assess the effect of baseline predictors.
RESULTS: 1782 CEAs (bilateral 142, mean age 71.4±9.3 years; 56.3%
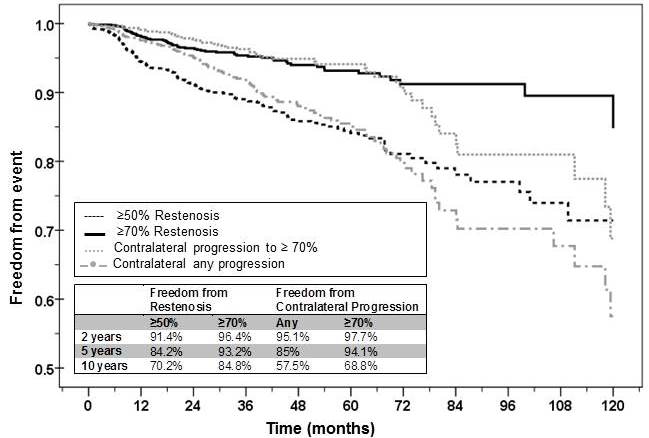
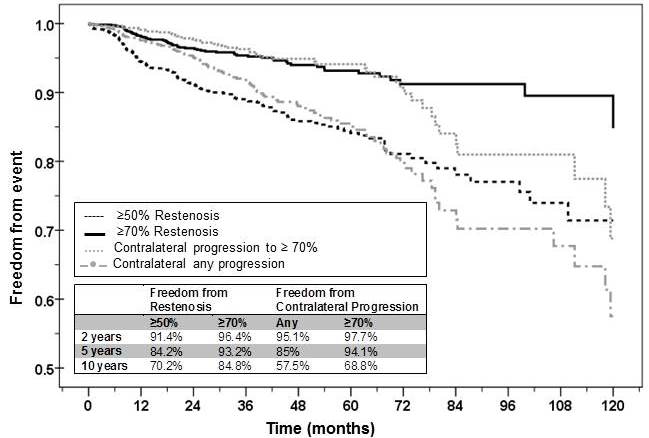
male; 35.4% symptomatic, 2.7% combined CABG) were performed during the study period with a mean clinical follow up of 54.8 months (1-155 months). Periprocedural stroke and death rates were 1.9% and 0.8% respectively (stroke/death: overall 2.6%, asymptomatic cohort 1.8%).Freedom from restenosis and contralateral carotid stenosis progression is shown in Figure 1, both events attaining higher rates of critical values (≥70%) after 5 years. Thirty one (20.4%) restenosis were symptomatic (5 at ≥50%, 26 at ≥70%) and 40 (26.3%) underwent reintervention. Restenosis was predicted by hypertension (HR 2.06, p=.031), female gender (HR 1.54, p=.012) and younger age ≤65 (HR 1.64, p=.009); contralateral progression was predicted by smoking (HR 1.85, p=.007) and renal insufficiency (HR 2.40, p=.001) resulting in carotid intervention in 27.1% of patients. No association was shown with either closure technique (primary vs patch vs eversion) or statins.Any stroke (118 events, 68 ipsilateral, 49 contralateral) rates at 5 and 10 years were 7.2% and 14.9% respectively. Predictors were symptomatic indication (HR 1.51, p=.033), renal insufficiency (HR 1.58, p=.046) and no statin use (HR 3.41, p=.006) at baseline. The rate of stroke referable to contralateral progression was 5.6% (6/107).
CONCLUSIONS: Restenosis and contralateral carotid stenosis following CEA progress significantly after 5 years, with possible impact on surveillance strategies. Restenosis was not associated with closure technique. Statin use reduces new symptoms but not the rate of disease progression.
Back to Annual Meeting Symposium

|