Back to Annual Meeting Symposium
Impact of early and delayed post-op myocardial infarction on late survival in patients undergoing vascular surgery
Virendra I. Patel, MD MPH, Emel Ergul, MS, Robert T. Lancaster, MD MPH, Glenn M. LaMuraglia, MD, Christopher J. Kwolek, MD, Richard P. Cambria, MD, Mark F. Conrad, MD MSSc.
Massachusetts General Hospital, Boston, MA, USA.
Objective: Perioperative MI has been shown to increase early and late mortality following vascular surgical (VS) procedures. We evaluated the frequency and timing of MI after VS and its impact on survival across a heterogeneous cohort of VS patients.
Methods: All patients undergoing a spectrum of VS (open aortic resection, EVAR/TEVAR, CEA/CAS, or lower extremity bypass) from 7/2007 – 5/2012 were included and MI was diagnosed by EKG changes, elevated troponin, or diagnosis by a cardiologist. Patients were identified by CPT code using an institutional patient data research registry comprised of administrative/clinical data and stratified according to the temporal relationship of the MI to the indexed procedure (early = within 30 days, intermediate = 1month to 1year and late = >1 year). Univariate and multivariate methods were used to identify predictors of MI and its impact on survival.
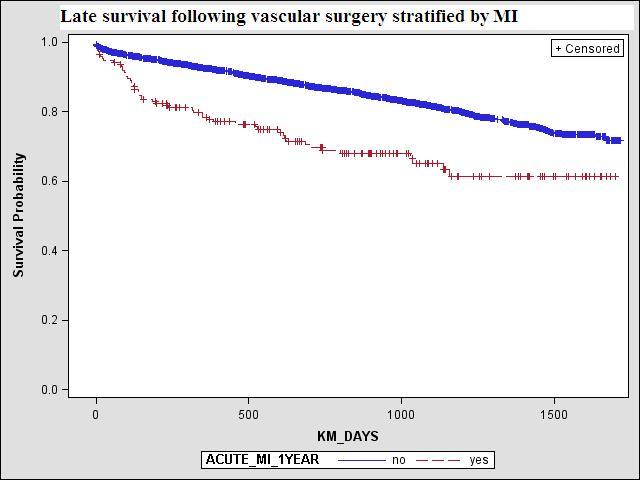
Results: We identified 2984 patients who underwent VS during the study interval. Early MI was observed in 110 (3.7%), intermediate MI in 66 (2.2%), and late MI in 136 (4.5)%. Patient age (per yr.) (OR1.02 [95%CI:1.0002–1.05]; P=0.03) and history of CAD (OR4.6 [95%CI:2.8–7.5]; P<0.01) independently predicted risk of early MI. Intermediate MI was predicted by history of CAD (OR3.2 [95%CI:1.9–5.3]; P<0.01) and diabetes (OR1.7 [95%CI:1.1–2.7]; P=0.02). Procedure type was not predictive of peri-op or delayed MI. Patients having an MI within the first year had a lower (Log rank P<0.001) survival at one (77±3% 1yr. vs. 92±1%) and five years (61±5% vs. 71±2%) (Figure1). Risk adjusted (age, gender, CAD, race, HTN) Cox regression modeling showed that early MI (HR1.5 [95%CI:1.01–2.2]; P=0.04) and more importantly intermediate MI (HR2.2 [95%CI:1.5–3.2]; P<0.01) independently predicted increase in late mortality, while late MI had no impact (HR1.03 [95%CI:0.7–1.6]; P=0.9).
Conclusions: Incidence of MI within the first year after major vascular procedures remains low, yet is predicted by a history of CAD and diabetes. Readily indentifiable high risk should have focused intensive medical therapy before and after VS.
Back to Annual Meeting Symposium

|

