|
|
 |
Back to Annual Meeting Symposium
Outcomes of Lower Extremity Revascularization (LER) in Patients on Dialysis
Justin Wallace, MD, Joseph Sidaoui, MD, Larry Fish, PhD, Luke Marone, MD, Donald Baril, MD, Efthimios Avgerinos, MD, Michel Makaroun, MD, Rabih A. Chaer, MD.
University of Pittsburgh, Pittsburgh, PA, USA.
OBJECTIVES: Dialysis patients with peripheral vascular disease (PVD) are at high risk for complications following surgical bypass, and it is not clear if endovascular interventions have affected survival and limb salvage in this patient population. We sought to characterize the outcomes of endovascular and open revascularization in dialysis patients treated for claudication or critical limb ischemia (CLI).
METHODS: The United States Renal Data System (USRDS) was utilized to review all patients undergoing LER in dialysis patients in the United States between 2005-2008. Diagnoses and procedures were identified by ICD-9 and CPT codes respectively. Primary outcomes were mortality and limb salvage. Bivariate associations were tested using the chi-squared test, and predictors were identified using Cox regression models.
RESULTS: A total of 12,029 incident dialysis patients underwent LER (24% endo,76% open). CLI was the indication in 79.9% of endo LER, and 72.8% of open LER. Major amputation rate within 30 days for CLI patients was 15.1% (15.7% endo,13.1% open, p=.002), and for claudicants was 5.2% (5.2% endo,4.9% open, p=.771). At 1 year, 32.0% of CLI patients (33.0% endo,29.1% open, p<0.001), and 14.4% of claudicants (14.0% endo,16.4% open, p=.254) had undergone major amputation.
The mortality rate at 30 days for CLI patients was 7.8% (7.2% endo,9.8% open, p=.001), and for claudicants was 5.2% (4.7% endo,7.9% open, p=.018). At 1 year the mortality rate was 38.4% for CLI patients (37.6% endo,40.9% open,p=.005) and 25.7% for claudicants (25.7% endo,25.2% open, p=.820).
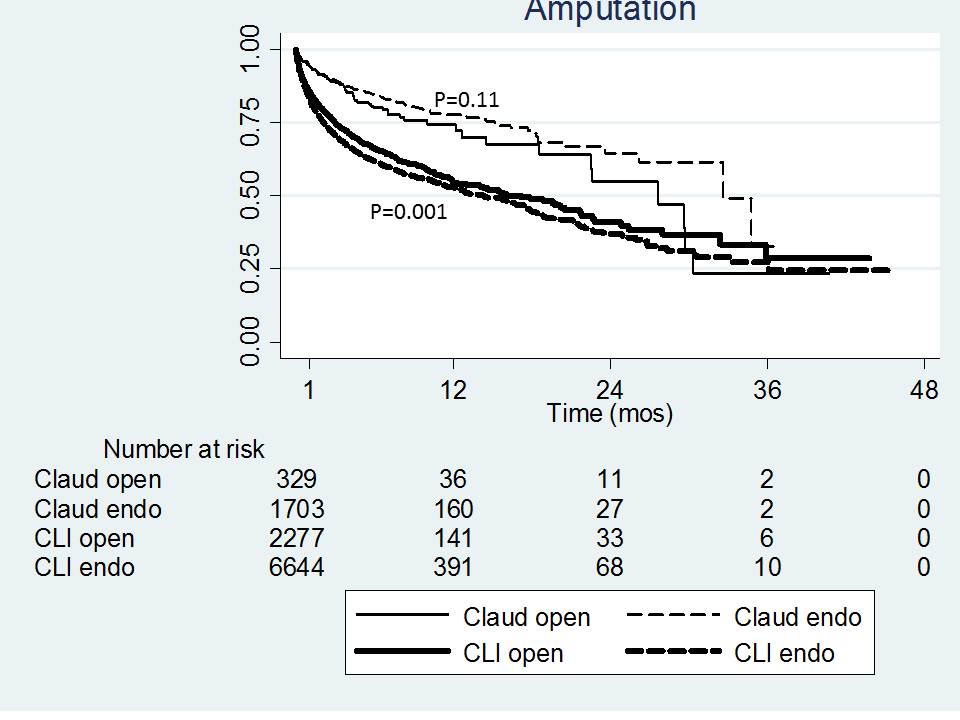
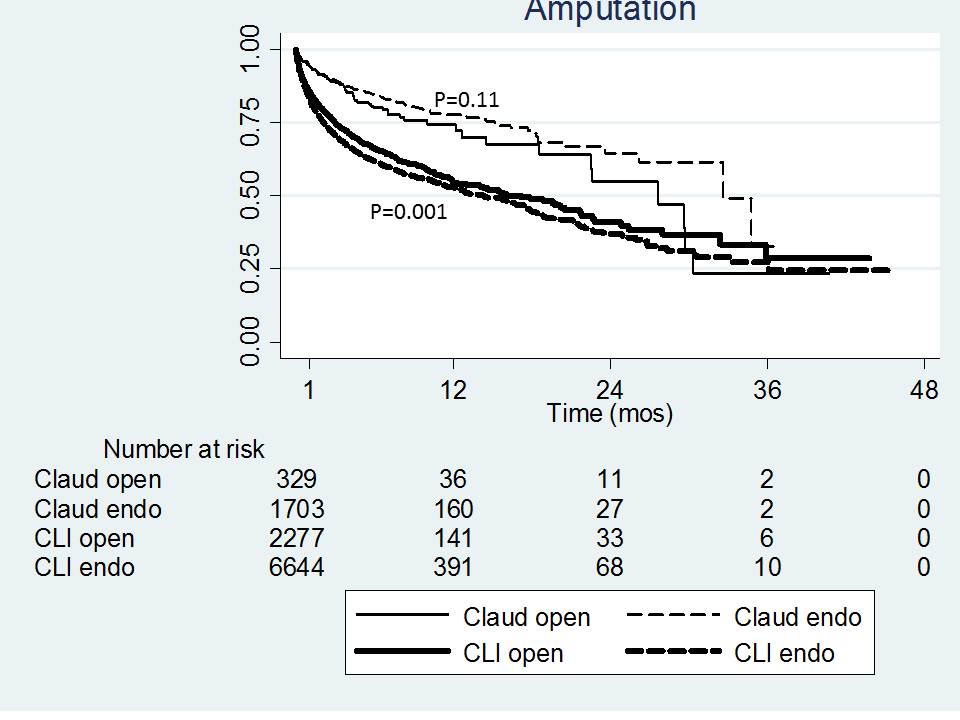
There were no significant differences between estimated survival for endo and open procedures at 1 year when stratified by clinical indication. Estimated limb salvage differed significantly between open and endo LER only among CLI patients, with open LER associated with improved limb salvage (p=.001) (Figure). Significant predictors of post-LER mortality were older age (p<.001) and congestive heart failure (p<.001).
CONCLUSIONS: Mortality and amputation rates following LER for dialysis patients are significant, particularly for patients with CLI. Although open LER is associated with improved limb salvage compared to endo LER, mortality is greater at 30-days and 1-year. Given the high overall mortality rates, the presence of dialysis-dependence questions the indication for LER, especially for claudication.
Back to Annual Meeting Symposium

|