|
|
 |
Back to Annual Meeting Symposium
Long-term Results for Primary Bypass versus Primary Angioplasty/Stent for Lower Extremity Critical Limb Ischemia
Jeremy D. Darling, B.A., Lindsey Korepta, M.D., Thomas Curran, M.D., John C. McCallum, M.D., Dominique Buck, M.D., Elliot L. Chaikof, M.D., Raul J. Guzman, M.D., Mark C. Wyers, M.D., Allen Hamdan, M.D., Marc L. Schermerhorn, M.D..
Beth Israel Deaconess Medical Center, Boston, MA, USA.
OBJECTIVES:
Long-term results comparing percutaneous transluminal angioplasty ± stent (PTA/S) and surgical bypass (BPG) for critical limb ischemia (CLI) in patients who have had no prior intervention have not been extensively reported. We detail our results with 3-year follow-up.
METHODS:
We reviewed all lower extremity revascularization procedures at our institution from January 2005 to December 2010, where 927 patients presented for CLI and underwent a first time intervention. Outcomes included complications, restenosis, symptom recurrence, reinterventions, minor and major amputations and mortality. Predictors for reintervention and amputation were identified using a Cox regression model.
RESULTS:
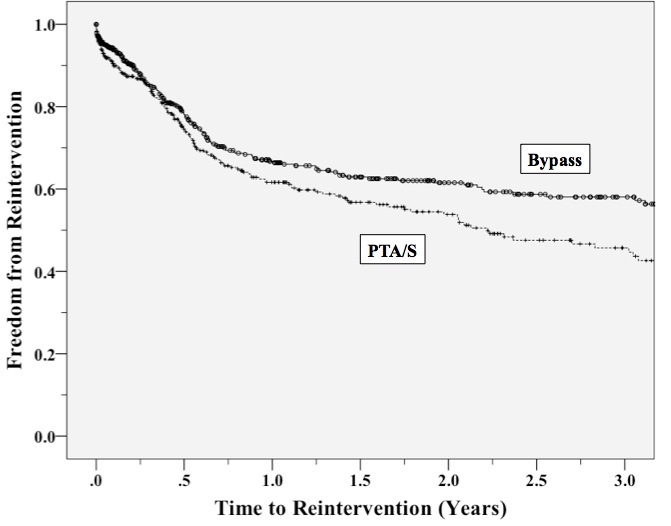
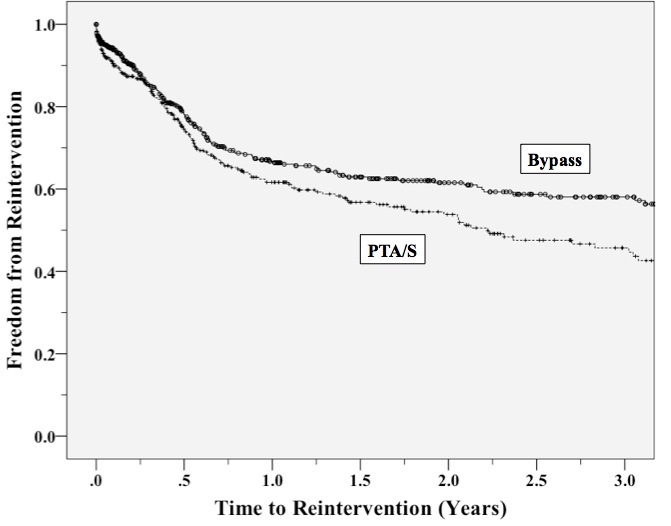
Of the 927 patients, 519 underwent BPG and 408 underwent PTA/S. BPG were above the knee in 58% (40% vein) and below the knee in 42% (100% vein). Mean age was 70.5 (BPG) versus 72.4 (PTA/S; P = .03), with more males undergoing BPG (64% vs. 52%; P<.01). Mean length of stay (LOS) was 10 days (BPG) versus 7.4 days (PTA/S; P =.02), with 3-year reintervention rates significantly lower in patients undergoing BPG (42% vs. 54%; P<.01). There were no differences in perioperative mortality (3% vs. 2%; not significant [NS]). Wound infection was 11% in BPG patients; however, BPG showed improved freedom from restenosis (78% vs. 67% at 3 years; odds ratio [OR], 1.6; 95% confidence interval [CI], 1.2-2.1). A Cox regression model of all patients showed that a reintervention within 3 years was predicted by PTA/S (OR, 1.6; 95% CI, 1.1-2.3) (see Figure) and a history of smoking (OR, 1.3; 95% CI, 1.0-1.6). Major amputations were predicted by gangrenous indications (OR, 1.9; 95% CI 1.1-3.5) and were not predicted by procedure type.
CONCLUSIONS:
BPG for the primary treatment of critical limb ischemia showed improved freedom from restenosis and significantly fewer reinterventions than PTA/S within 3 years, but was associated with increased LOS and wound infection. Perioperative mortality and 3-year amputation rates were similar between procedure types.
Back to Annual Meeting Symposium

|