Back to Karmody Posters
Implementation of best medical therapy for cardiovascular risk factors in vascular surgery patients
Mark E. O'Donnell, MMedSc MD FRCS, Damian McGrogan, MB MRCS, David Mark, MB MRCS, Bernard Lee, FRCS.
Belfast City Hospital, Belfast, United Kingdom.
OBJECTIVES: Current clinical evidence reports that antiplatelet, statin, angiotensin converting enzyme inhibitor and beta blockade therapies have advantageous effects on vascular surgery patient morbidity and mortality. Unfortunately, such patients appear to be less likely to receive optimal medical management when compared to coronary artery disease patients. This study assessed medical therapy prescribing in patients attending a regional vascular surgery unit.
METHODS: A retrospective review between February 2010 and February 2011 was performed for patients undergoing aortic aneurysm, carotid, peripheral arterial and amputation surgeries. Gender, age, smoking history, body mass index and cardiovascular risk factors were documented from inpatient charts. Current admission medications and subsequent modification by the vascular team were recorded.
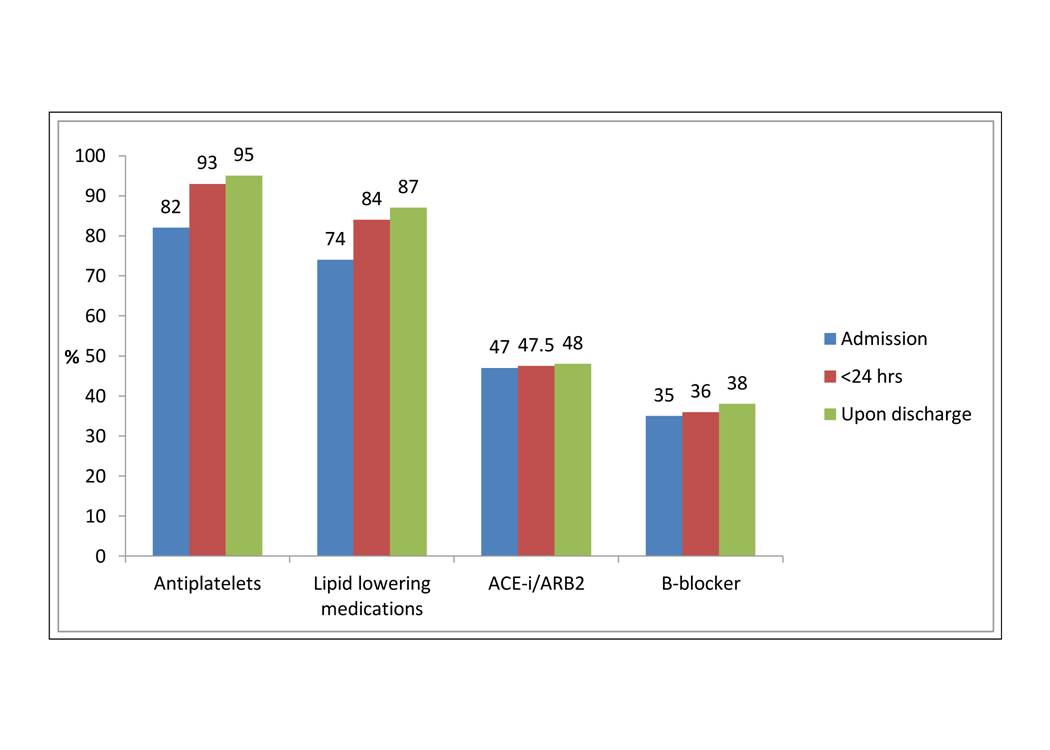
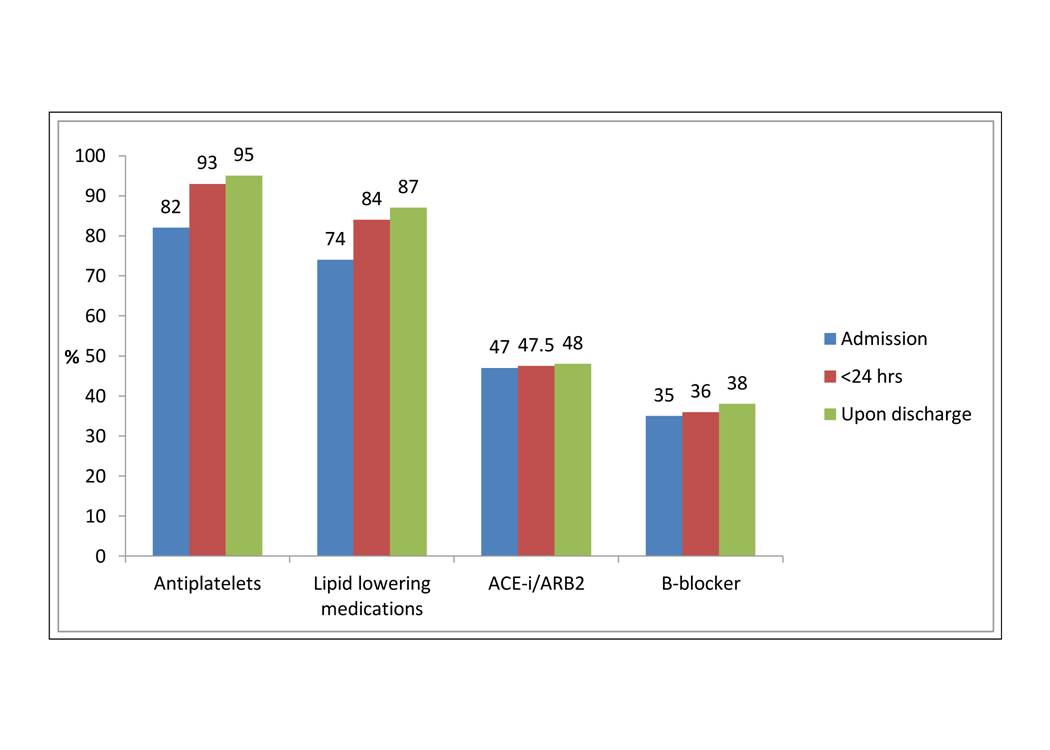
RESULTS: Two hundred and forty-four patients (male=165, mean age=71 years) were identified. Prevalence of hypertension, hypercholesterolemia, myocardial infarction, angina, stroke and diabetes were significantly higher than in the general age-matched population. 201 (82.3%) patients were on antiplatelet or antithrombotic medication upon admission to the vascular ward which was improved to 231 (94.6%) patients on discharge. 180 (73.7%) patients were on lipid lowering therapy upon admission which improved to 213 (87.2%) patients on discharge. A total of 115 (47.1%) patients were on ACE-inhibitor or angiotensin 2 receptor blocker medications on admission and this was improved to 118 (48.3%) upon discharge. 87 (35.6%) patients were on a beta blocker which improved to 93 (38.1%) patients upon discharge.
CONCLUSIONS: Implementation of best medical therapy is widely adopted in the community with compliance rates greater than 73% for aspirin and statin therapy. Vascular surgeons should remain vigilant for further opportunities to optimise medical therapy in this high risk patient group particularly in antithrombotic, lipid lowering and antihypertensive therapies.
Figure 1: Medication demographics with percentage of patients prescribed antiplatelet, lipid lowering, angiotensin converting enzyme inhibitors / receptor blockers and beta-blocker therapies on admission, within 24-hours of admission and within 24-hours prior to discharge (n=244).
Back to Karmody Posters

|