|
|
 |
Back to Karmody Posters
Mid-term Cost Analysis of Endovascular versus Open Repair in the Treatment of Thoracic Aortic Aneurysms
Jacob R. Gillen, MD, Basil W. Schaheen, MD, Kenan W. Yount, MD, MBA, Margaret C. Tracci, MD, JD, Gorav Ailawadi, MD, Saher S. Sabri, MD, John A. Kern, MD, Irving L. Kron, MD, Gilbert R. Upchurch, Jr., MD, Christine L. Lau, MD, MBA.
University of Virginia Health System, Charlottesville, VA, USA.
Objective:
For descending thoracic aortic aneurysms (TAAs), endovascular stents (TEVARs) reduce operative morbidity and mortality compared to open surgical repair. However, long-term differences in patient survival have not been demonstrated, and an increased need for aortic reintervention has been observed. This study investigated mid-term outcomes and hospital costs of TEVAR compared with open TAA repair.
Methods:
This was a retrospective, single institution review of elective thoracic aortic aneurysm repairs between 2005 and 2012. Patient demographics, operative outcomes, reintervention rates, and hospital costs were assessed. The literature was also reviewed to determine commonly observed complication and reintervention rates for TEVAR and open repair. Monte Carlo simulation was utilized to model and forecast hospital costs for TEVAR and open TAA repair at 30 days and 3 years.
Results:
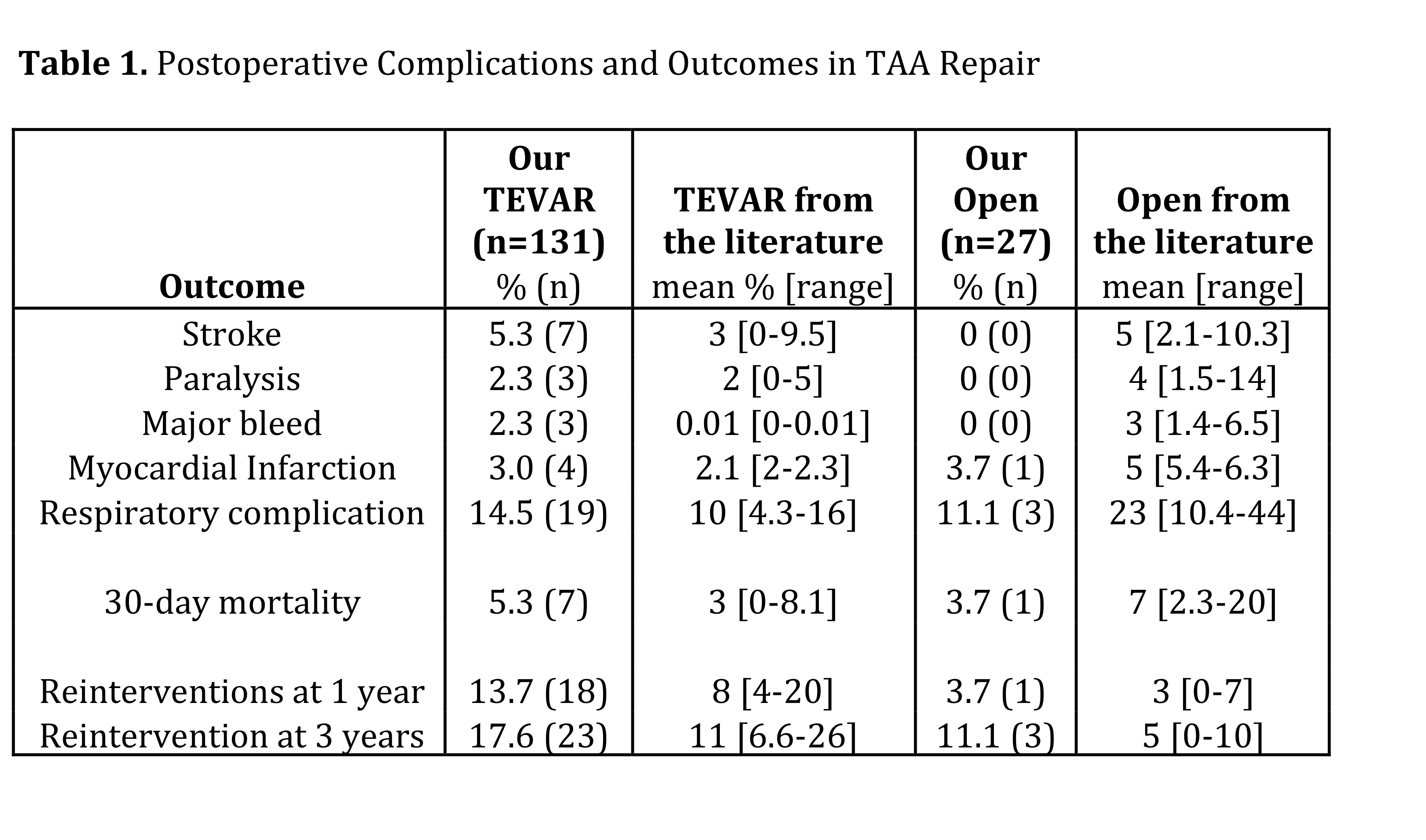
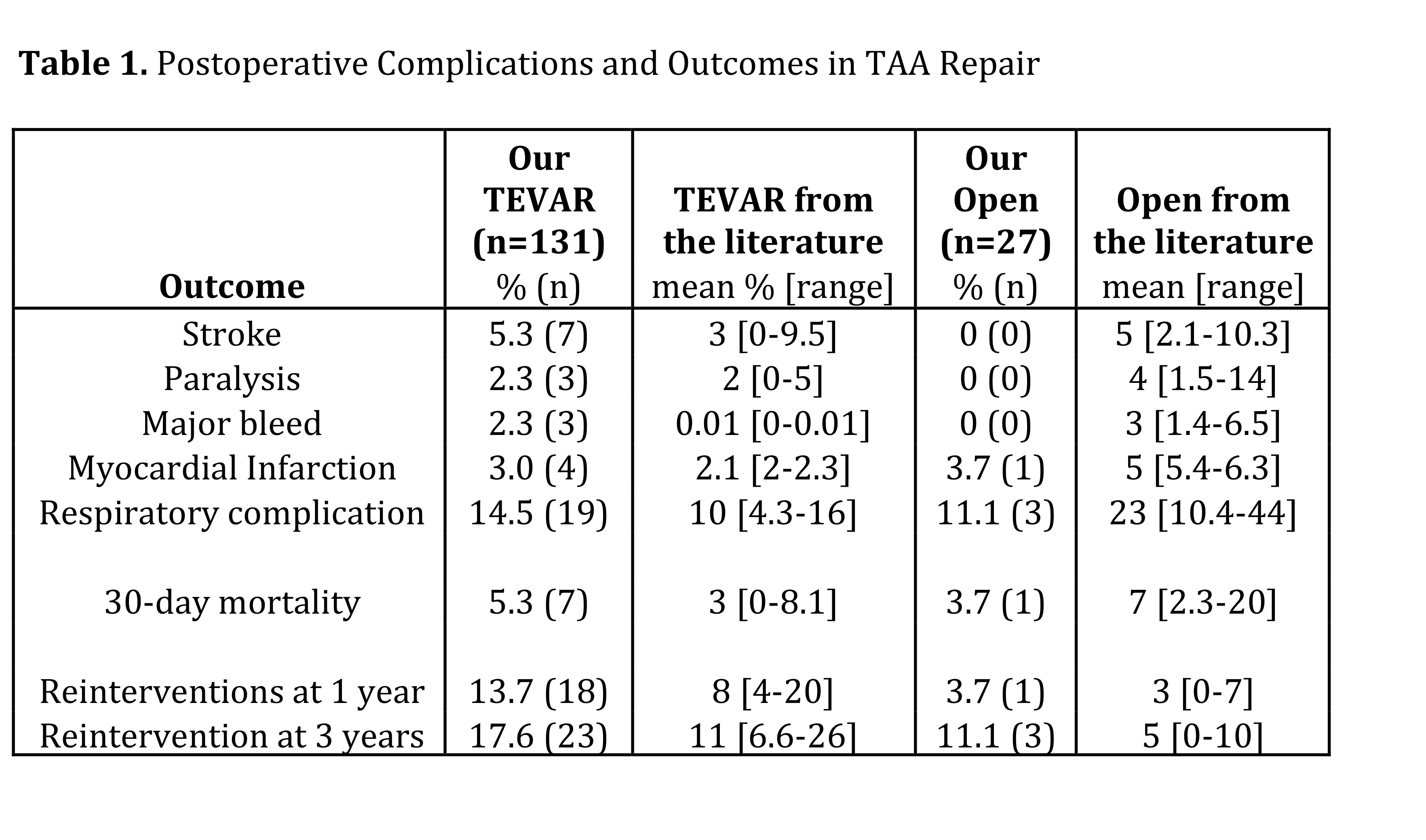
Our cohort consisted of 131 TEVARs and 27 open repairs that were well matched demographically. Operative mortality for TEVAR and open repair was 5.3% and 3.7%, respectively (p=1.0). There was a trend towards more complications in the TEVAR group, although not statistically significant (all p>0.05, Table 1). Hospital costs were significantly greater in the TEVAR group ($52,008 vs $37,172, p=0.001). However, cost modeling utilizing reported complication and reintervention rates from the literature [Table 1] overlaid with our cost data produced a higher cost for the open group at 30 days ($55,119 vs $48,163) and at 3 years ($58,655 vs $52,638). Interestingly, TEVAR hospital costs, not reintervention rates, were the most significant driver of cost in the TEVAR group.
Conclusions:
Our institution’s data showed higher costs with TEVAR compared to open TAA repair due to the small number of complications within the open group. This relationship was reversed in our cost model, with higher costs in the open group at both 30 days and 3 years. These findings reinforce that single institution data can be deceptive compared to multi-institutional trends. Cost modeling is one method that may provide more accurate and generalizable information for comparisons between various intervention options.
Back to Karmody Posters

|