|
|
 |
Back to Annual Symposium Program
Multi-disciplinary care pathways predict amputation-free survival in chronic critical limb ischemia
Jayer Chung, MD, David A. Timaran, MD, J Gregory Modrall, MD, Lawrence A. Lavery, DPM, MPH, Carlos H. Timaran, MD, Mirza S. Baig, MD, Melissa L. Kirkwood, MD, R James Valentine, MD.
University of Texas Southwestern Medical Center, Dallas, TX, USA.
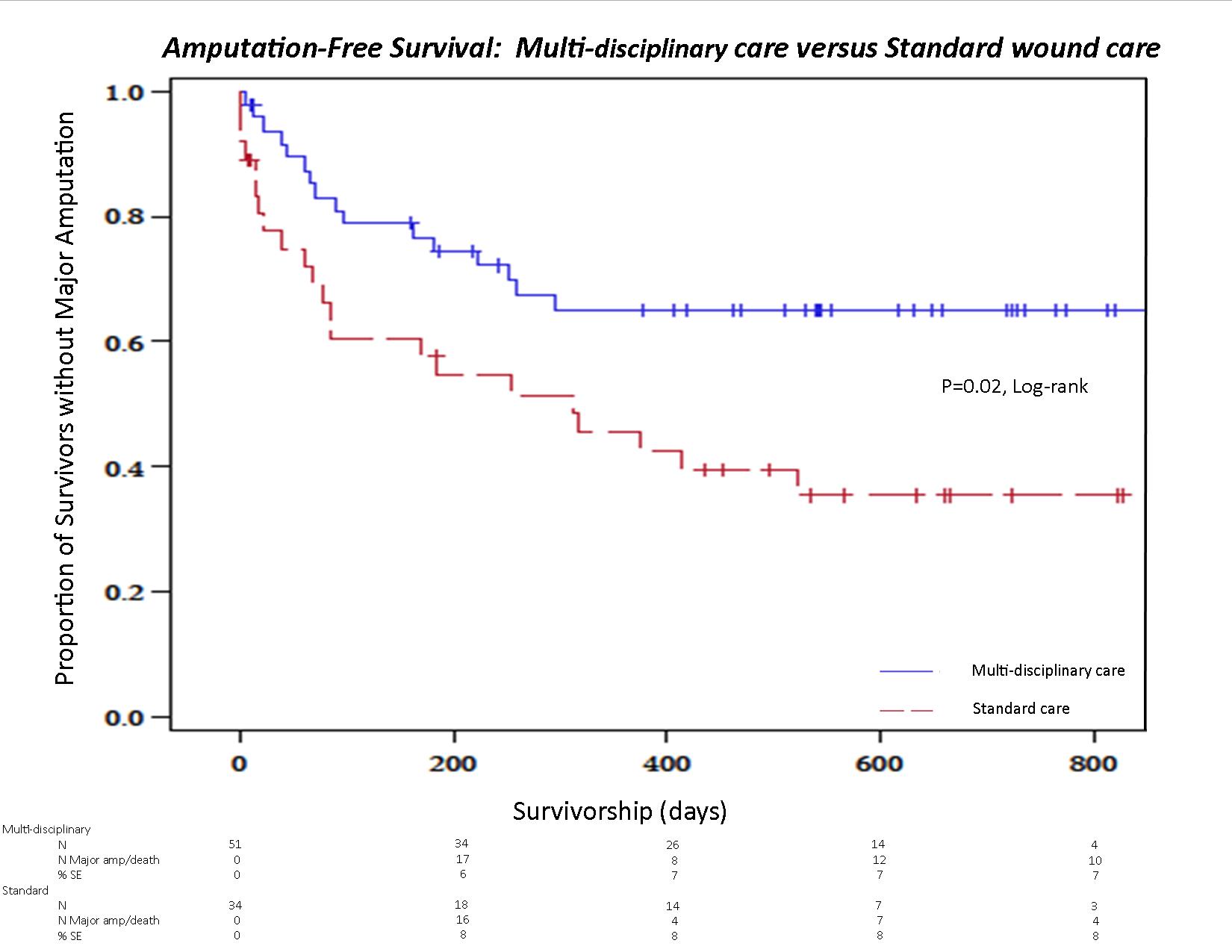
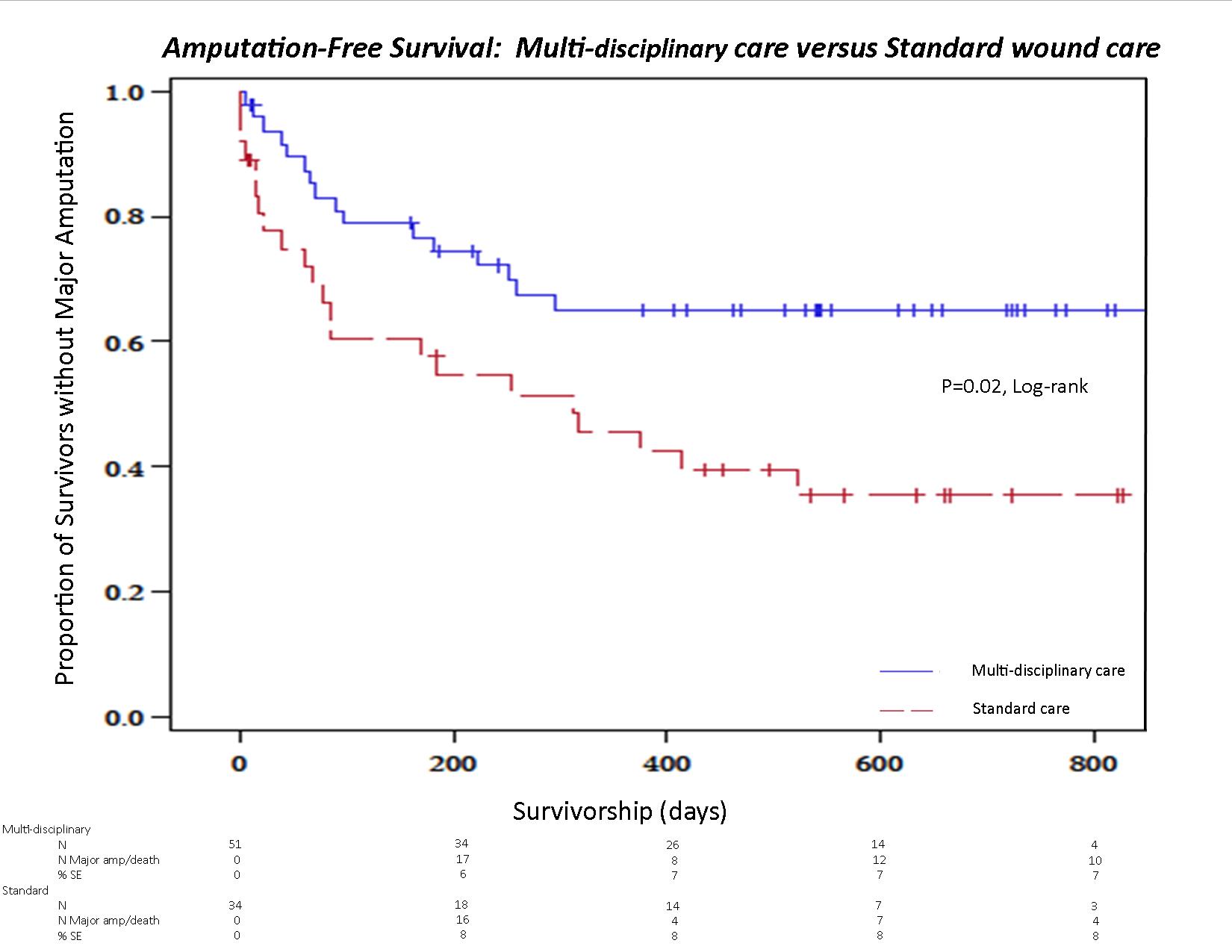
Objective: Quantify the effect of multi-disciplinary care upon amputation-free survival (AFS), and wound healing among chronic critical limb ischemia (CLI) patients.
Methods: We retrospectively reviewed a single-center, prospectively maintained database of consecutive, CLI patients presenting to the Vascular Surgery service. Subjects who received initial and follow-up
wound care from the multi-disciplinary team (MWC; Vascular Surgery, Plastic Surgery and Podiatric Surgery), were compared to patients who received standard wound care (SWC; heterogeneous mixture of nurses, General Surgeons, internists and/or the patients themselves). Allocation
of patients to either arm was determined by the referring physician or
attending vascular surgeon at the time of consultation. The primary outcome variable is AFS. Significant univariate predictors of AFS and wound-healing were entered into a multivariate Cox proportional hazards model and assessed at an α=0.05.
Results: Between August, 2010 and June, 2012, 145 patients (91 male, 63%) with CLI were evaluated by the Vascular Surgery Service with a median follow-up of 539 (IQR 314, 679) days. 85 subjects presented with ischemic tissue loss (N=39; Rutherford category 5; N=46, Rutherford category 6). Within this cohort 60% (N=51) had MWC, and 40%
(N=34) had SWC. 59 (69%) subjects underwent revascularization (34=endovascular, N=18=open, 7=hybrid), 11 (13%) were managed with primary major amputation. 15 (18%) declined intervention. AFS (mean, +/- se) was superior for the MWC arm (593 +/- 53.5 versus 281 +/- 38.2 days; HR=2.14, 95% CI, 1.14, 4.04; p=0.02, Χ2). Wound-healing (mean +/- se) favored the MWC arm (426.1 +/- 31.1 versus 610 +/- 91 days), which was not statistically significant (HR=1.33; 95% CI, 0.54, 3.28; p=0.53, Χ2). Multivariate analysis revealed the following independently predicted AFS: revascularization (HR=2.94; 95% CI 1.48, 5.84; p<0.01, Χ2); treatment by the MWC (HR=1.99; 95% CI 1.23, 3.21; p<0.01); and baseline independent ambulation (HR=2.40, 95% CI 1.60, 3.60; p<0.01).
Conclusions: Multi-disciplinary care for CLI patients durably improves AFS by a factor of two, and should be the standard of care for the CLI population. Wound healing remains prolonged regardless of pre-operative or post-operative wound care. Future study is required to evaluate the
costs and functional outcomes for MWC for CLI patients.
Back to Annual Symposium Program

|