|
|
 |
Back to Annual Symposium Program
Use of Antiplatelet Agents in Patients Receiving Lower Extremity Endovascular Interventions: A Regional Review of Compliance and Outcomes
Lily E. Johnston, MD1, Megan Tracci, MD1, Patrick A. Stone, MD2, Ali AbuRahma, MD2, David V. Strider, PhD1, Mary Baldwin1, Gilbert R. Upchurch, Jr., MD3.
1Department of Surgery, University of Virginia, Charlottesville, VA, USA, 2Department of Surgery, Robert C. Byrd Health Sciences Center, West Virginia University, Charleston, WV, USA, 3Department of Surgery, University of Virginia, on behalf of the Virginias Vascular Study Group, Charlottesville, VA, USA.
OBJECTIVES: The American College of Chest Physicians has recommended that all patients with peripheral arterial disease (PAD) be on a single agent antiplatelet regimen for secondary prevention unless contraindicated, and that patients undergoing percutaneous transluminal angioplasty (PTA) be maintained on long-term single agent antiplatelet therapy. The purpose of this study was to evaluate regional compliance with these guidelines, and to further characterize patterns of noncompliance with respect to outcomes.
METHODS: De-identified data were provided by the Virginias Vascular Study Group, which maintains a clinical vascular surgery database including patients in Virginia and West Virginia. Inclusion criteria were angioplasty and/or stent of a proximal lower extremity vessel (iliac through femoral). Patients requiring emergent intervention were excluded. We examined the records for patient characteristics pre-procedure as well as follow-up data post-procedure. Data were analysed using IBM SPSS Statistics, version 19. Hazard functions were plotted where appropriate; these were tested with a log-rank test.
RESULTS: Of 1,060 records available, 814 met inclusion criteria. Over 25% of patients were not on aspirin at the time of their intervention, and just under 20% were on no antiplatelet therapy of any kind. Medical contraindication to antiplatelet therapy accounted only for approximately 1% of patients. The majority of patients were discharged on appropriate medical therapy: only 2.6% of patients were discharged without either aspirin or a P2Y12 inhibitor. Hazard functions for time to percutaneous and surgical re-intervention, respectively were plotted for patients based on their antiplatelet regimen at the time of their initial intervention. Patients on antiplatelet therapy have fewer overall re-interventions and those interventions happen later than patients who were not on antiplatelet therapy at the time of their procedure.
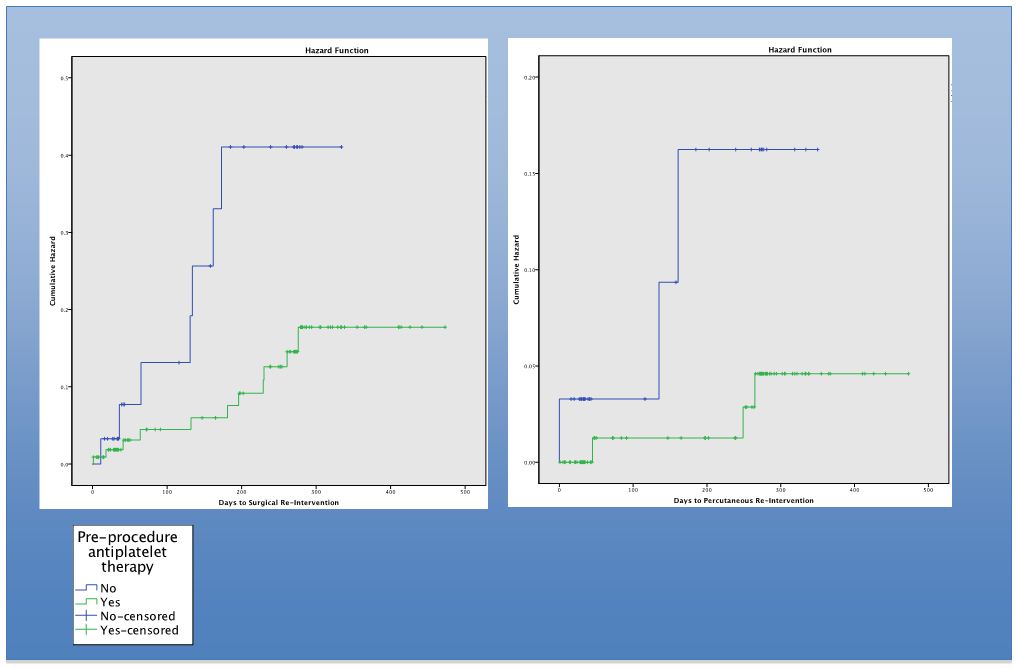
CONCLUSIONS: A single antiplatelet strategy for optimizing PAD patients preoperatively has not been agreed upon, but our data indicate suboptimal compliance with existing guidelines regarding medical management of PAD. These data also suggest that improving compliance with antiplatelet therapy could delay and possibly prevent the need for re-intervention in this population.
Back to Annual Symposium Program

|

