Back to Annual Symposium Program
Perioperative Management of Antiplatelet Therapies in Patients with Coronary Stents: Significant Differences Between Vascular and Non-Vascular Surgeons
Arman Kilic, Ibrahim Sultan, James H. Black, Thomas Reifsnyder.
Johns Hopkins Hospital, Baltimore, MD, USA.
OBJECTIVES: An increasing number of patients undergoing non-cardiac surgery have coronary stents. Although guidelines regarding perioperative management of antiplatelet therapies in this patient population exist, practice patterns remain incompletely understood. This study evaluated these practice patterns, with particular attention to differences in management between vascular and non-vascular surgeons.
METHODS: A link to a 23-question survey was displayed in the American College of Surgeons (ACS) electronic newsletter NewsScope, which is posted on the ACS website and emailed to 45,000 members. Questions were focused on perioperative management of antiplatelets (aspirin, clopidogrel) for bare-metal (BMS; placed within 2 months) and drug-eluting stents (DES; placed within the past year) during low and high-risk bleeding procedures, assuming a patient with no other confounding medical issues. Primary stratification was by surgeon specialty.
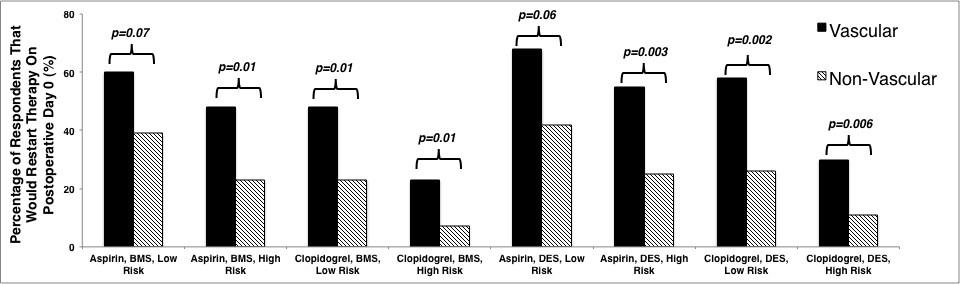
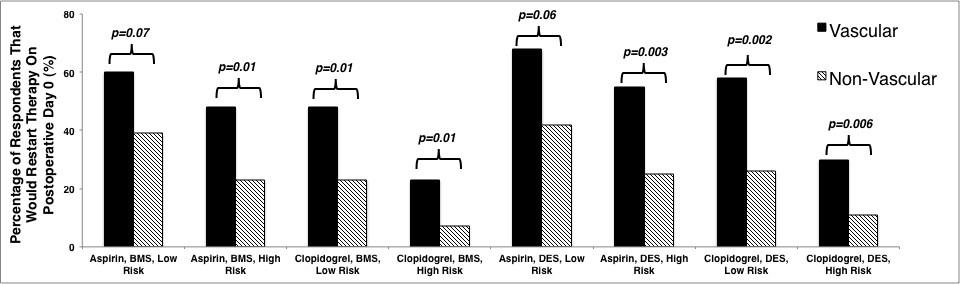
RESULTS: A total of 244 surgical providers responded to the survey, of which 40 (17%) were vascular surgeons. The majority of respondents were attending surgeons in practice for at least ten years (n=190; 79%). A significantly higher percentage of vascular versus non-vascular surgeons would not stop aspirin preoperatively in low bleeding risk procedures (BMS: 90% versus 54%, p=0.001; DES: 88% versus 58%, p=0.009). A higher percentage of vascular surgeons would not stop aspirin preoperatively in high bleeding risk procedures as well (BMS: 70% versus 28%, p<0.001; DES: 78% versus 32%, p<0.001). Most vascular surgeons would not stop clopidogrel in a low risk BMS patient (53% versus 21% of non-vascular surgeons, p=0.001). Similar findings with clopidogrel were observed in low (would not stop: 65% vascular versus 30% non-vascular, p<0.001) and high-risk DES patients (would not stop: 30% vascular versus 8% non-vascular, p=0.001). The same trends were observed in resuming antiplatelets in the postoperative period (Figure). The majority of respondents were not familiar with professional guidelines regarding perioperative antiplatelet management (n=128; 52%), with no differences between vascular and non-vascular surgeons (45% versus 54%, p=0.30).
CONCLUSIONS: This national survey demonstrates significant variation in perioperative antiplatelet management in patients with coronary stents, with marked differences between vascular and non-vascular surgeons. More effective communication of existing guidelines, or the development of new specialty-specific professional guidelines appears prudent.
Back to Annual Symposium Program

|