|
|
 |
Back to Annual Symposium Program
Outcomes of Redo Aortobifemoral Bypass for Peripheral Arterial Occlusive Disease
Bradley Schmit, MD, Salvatore Scali, MD, Robert Feezor, MD, Adam Beck, MD, Catherine Chang, MD, Alyson Waterman, MD, Scott Berceli, MD, Thomas Huber, MD.
University of Florida, Gainesville, FL, USA.
Objective: Patients presenting with occluded aortobifemoral bypass(ABF) grafts are managed with a variety of techniques. Redo ABF(rABF) procedures are infrequently performed due to concerns about procedural complexity and morbidity. The purpose of this analysis is to compare mid-term results of rABF to primary ABF(pABF) for occlusive disease to determine if there are significant differences in outcomes.
Methods: Retrospective review was performed of all patients undergoing ABF for occlusive disease from 2002-2012. Nineteen rABF and 194 pABF cases occurred during that time period. Data for an indication and comorbidity-matched cohort of 19 elective pABF patients were collected for comparison to the rABF group. Primary end-points were 30-day and all-cause mortality. Secondary end-points were complication rates, amputation-free survival(AFS) and freedom from major adverse limb events(MALE).
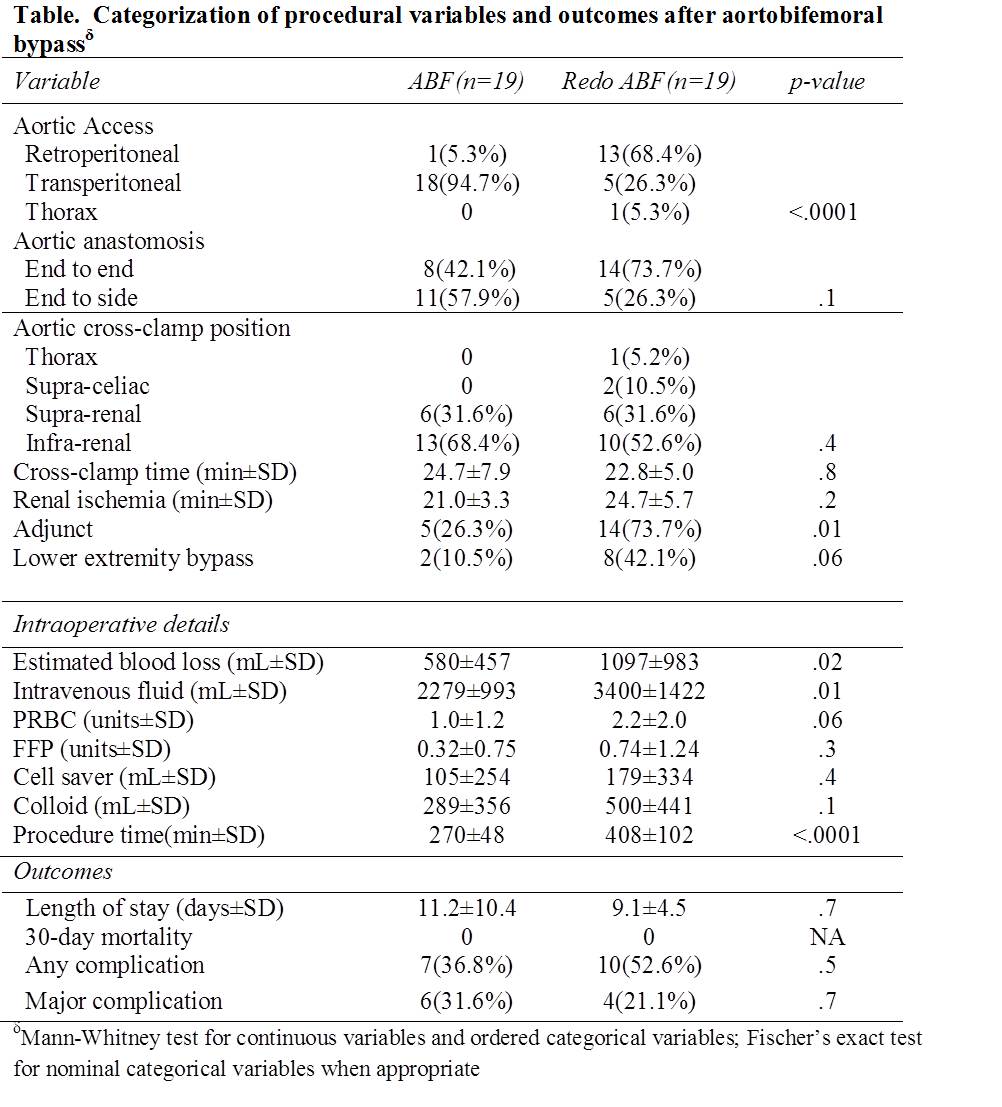
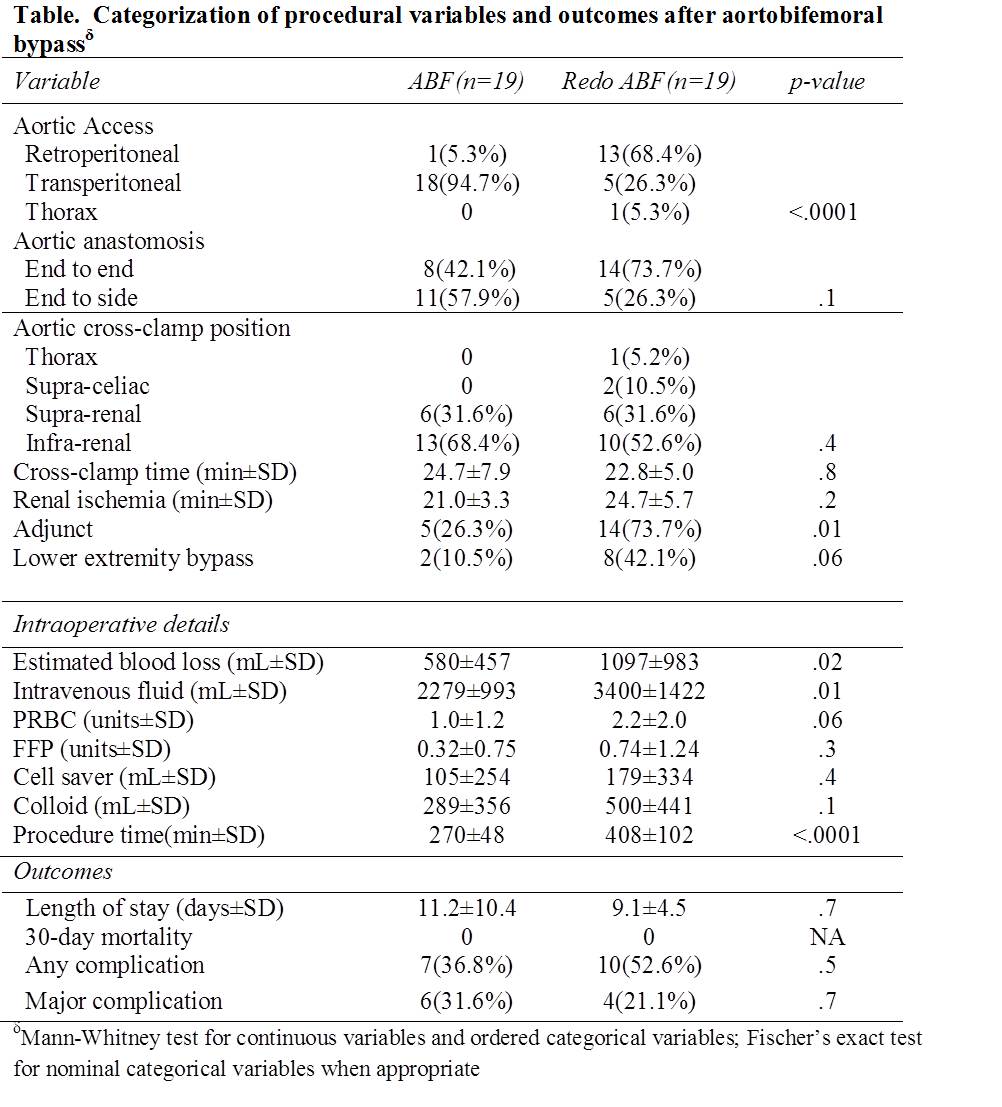
Results: rABF patients more frequently underwent prior extra-anatomic/lower extremity bypass operations compared to pABF(P=.02); however, no difference in prior failed iliac intervention(P=.4) was found. By design, indications for both rABF and pABF groups were the same: claudication, n=6/6(31.6%), P=1; critical limb ischemia, N= 13/13(78.4%), P=1. Aortic access was more frequently via retroperitoneal exposure in the rABF group(N=13 vs. N=1;P<.0001) and a significantly higher proportion of rABF patients required concomitant infrainguinal bypass or intra-procedural adjuncts such profundaplasty(N=14 vs. N=5;P=.01). Highlights of procedural differences are further depicted in the Table. Length of stay(days±SD) was similar (pABF, 11.2±10.4 vs. rABF, 9.1±4.5;P=.7) and no 30-day or in-hospital deaths occurred in either group. Similar rates of major complications occurred in the 2 groups[pABF, N=6 (31.6%) vs. rABF, N=4(21.1%)]; observed difference in rates, pABF-rABF=9.5%, 95% confidence interval (CI): -17.6-36.7%(P=.7).
Two-year survival(±standard error mean) was 91±9% and 90±9% for pABF and rABF patients(log-rank P=.8). Two-year AFS was 90±9% vs. 89±8% between pABF and rABF patients(log-rank, P=.5). Two-year freedom from MALE was 82±9% vs. 78±10% for pABF and rABF patients(log-rank, P=.6).
Conclusions: Patients undergoing rABF have higher procedural complexity as evidenced by greater operative time, blood loss and need for adjunctive procedures. However, similar perioperative morbidity, mortality and mid-term survival occurred in comparison to pABF patients. These results support a role for rABF in selected patients.
Back to Annual Symposium Program

|