|
|
 |
Back to Annual Symposium Program
Increasing Costs of Inpatient Care of Diabetic Foot Ulcers are Associated with Limb Salvage in Sicker Patients
Caitlin W. Hicks, MD, MS, Shalini Selvarajah, MD, MPH, Nestoras Mathioudakis, MD, Bruce A. Perler, MD, Julie A. Freischlag, MD, James H. Black, III, MD, Christopher J. Abularrage, MD.
The Johns Hopkins Hospital, Baltimore, MD, USA.
OBJECTIVES:
The cost of care for diabetic foot ulcers is estimated to be more than $1.5 billion annually. The aim of this study was to analyze inpatient diabetic foot ulcer cost changes over time and to identify factors associated with these costs.
METHODS:
The Nationwide Inpatient Sample (2005-2010) was queried using ICD-9 codes for a primary diagnosis of foot or ankle ulceration. The primary outcomes were changes in adjusted total hospital charges over time. Multivariable analysis was performed to assess relative increases (RI) in hospital charges per patient between 2005 vs. 2010 adjusting for demographics, income, comorbidities (Charlson Index≥3), insurance type, hospital characteristics, diagnostic imaging, revascularization, amputation, and length of stay.
RESULTS:
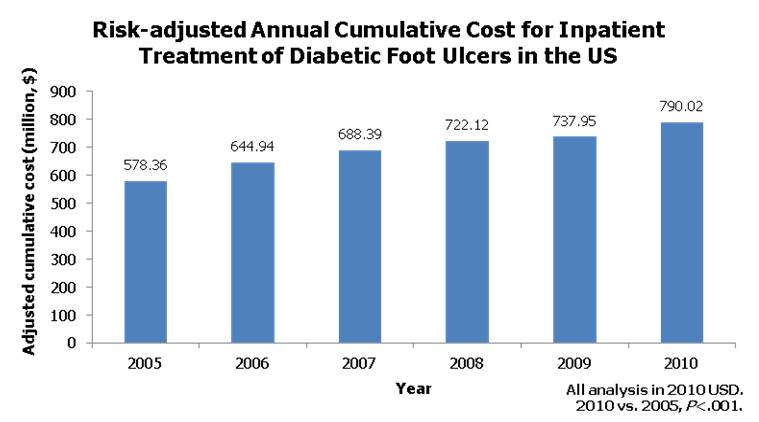
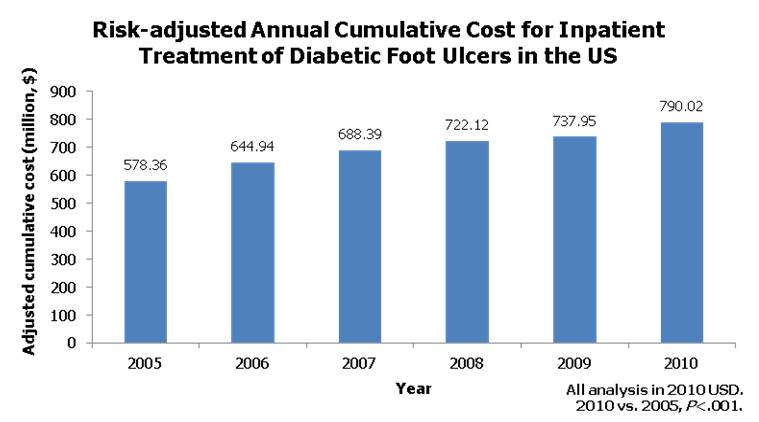
Overall, 336,641 patients were admitted with diabetic foot ulcers (mean age 62.9±0.1 years, 59% male, 61% white race). The annual cumulative cost for inpatient treatment of diabetic foot ulcers rose significantly from 2005 to 2010 ($578,364,261 vs. $790,017,704; Figure; P<0.001). More patients were hospitalized (128.6 vs. 152.8 per 100,000 hospitalizations; P<0.001), and the mean adjusted cost per patient hospitalization increased significantly over time ($11,483 vs. $13,258; P<0.001). The proportion of non-elective admissions remained stable (25% vs. 23%; P=0.32) and there were no differences in mean hospital length of stay (7.0±0.1 vs. 6.8±0.1; P=0.22). Minor (17.9% vs. 20.6%, P<0.001), but not major amputations (3.9% vs. 4.2%, P=0.27) increased over time. Based on multivariable analysis, the main factors contributing to the escalating cost per patient hospitalization included increased patient comorbidities (unadj. mean difference 2005 vs. 2010 $3,303 [RI:1.08] vs. adj. $15,220 [RI:1.35]), diagnostic angiography (unadj. $18,635 [RI:1.36] vs. adj. $29,079 [RI:1.46]), open revascularization (unadj. $15,145 [RI:1.25] vs. adj. $30,759 [RI:1.37]), endovascular revascularization (unadj. $17,662 [RI:1.29] vs. adj. $28.937 [RI:1.38]), and minor amputations (unadj. $9,918 [RI:1.24] vs. adj. $18,084 [RI:1.33])(P<0.001, all).
CONCLUSIONS:
Hospital charges related to diabetic foot ulcers have increased significantly over time despite stable hospital length of stay and proportion of emergency admissions. Risk-adjusted analyses suggest that this change may be reflective of a progressively sicker patient population, and increasing charges associated with diagnostic angiography and revascularization aimed at limb salvage. Despite this, overall major amputation rates remained stable.
Back to Annual Symposium Program

|