Back to Annual Symposium Program
Management and outcomes of failed revascularization using a selective endovascular-first strategy for critical limb ischemia
Karan Garg, MD, Rameen Moridzadeh, BS, Patrick A. Kaszubski, BS, Caron B. Rockman, MD, Mark A. Adelman, MD, Frank J. Veith, MD, Firas F. Mussa, MD.
NYU Langone Medical Center, New York, NY, USA.
OBJECTIVES: Patients with critical limb ischemia (CLI) remain at risk of significant limb loss despite timely intervention and reintervention. This study reports the fate of failed primary revascularization attempts and their rescued approaches.
METHODS: A cohort of 302 patients with CLI was identified between March 2007 and December 2010. Endovascular-first was selected if: 1) the patient had short (5-7cm occlusions or stenoses in crural vessels) 2) the disease in superficial femoral artery was limited to TASC II A, B or C and 3) no impending limb loss. Failures were defined as recurrent clinical signs and symptoms. Criteria for reintervention were the same as for primary intervention.
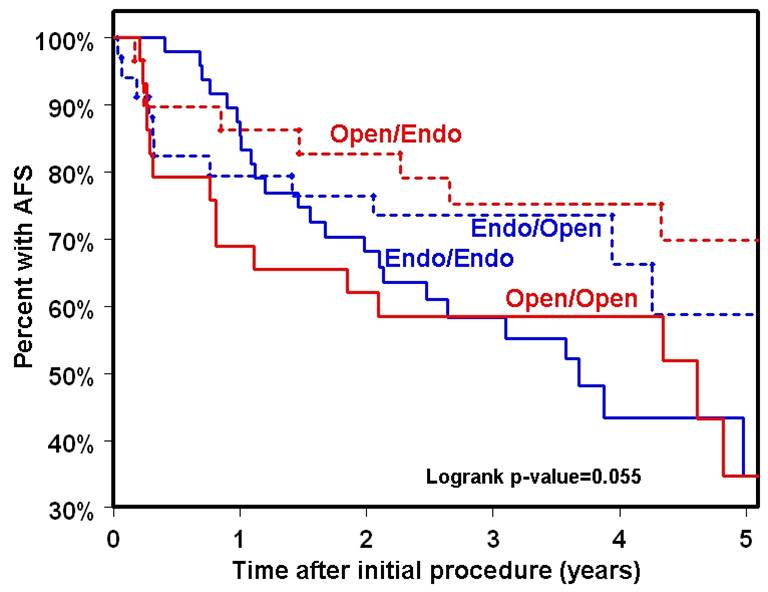
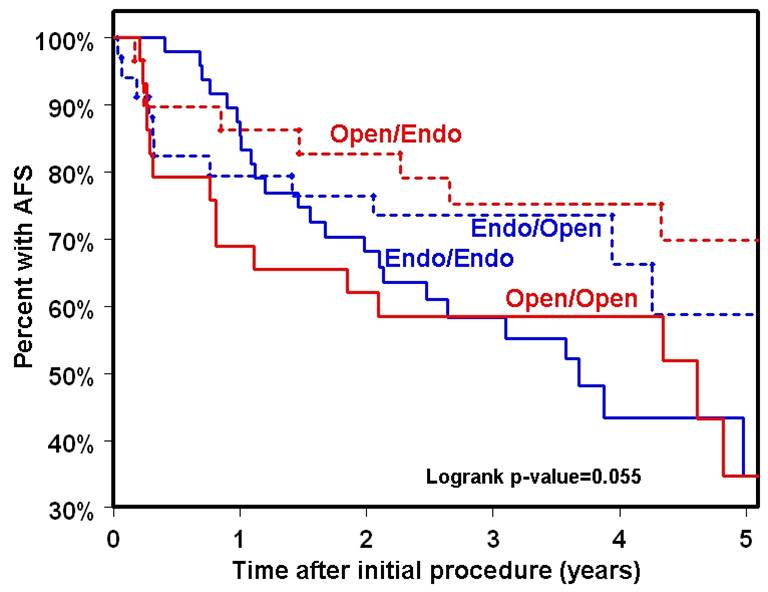
RESULTS: Endo-first was performed in 187 (62%) and open-first in 105 patients (35%). Secondary procedures (endo or open) were more common after open-first (68% vs. 55%; p= 0.029). Patients with above knee open-first intervention were less likely to undergo secondary interventions than those who underwent endo-first at same location, 58% versus 40% (p=0.003). Patients treated with rest pain were more like to undergo secondary interventions than those with ulcers, 29% versus 54% (p<0.0001). At five-years, mortality rates were higher among those without secondary interventions, 53% versus 39% (p=0.0096). However, amputation rates were higher in patients undergoing secondary interventions, 22% versus 5%, (p=0.0016). There was no difference in amputation free survival (AFS) based on need for secondary interventions, 49% versus 47%, (p=0.165) (Figure 1). Patients with an initial open intervention followed by endovascular reintervention had a trend towards the best outcome with 70% five-year AFS.
CONCLUSIONS: At 5 years, selective revascularization strategy led to frequent reinterventions, higher in those treated with an open-first approach. While amputation rates were higher in those undergoing secondary interventions, mortality was higher among those without secondary interventions. Amputation free survival was not different in the two cohorts with a trend towards improved outcomes in those undergoing an open-first followed by endovascular reintervention.
Back to Annual Symposium Program

|