|
|
 |
Back to Annual Symposium Program
Comparison of Patency Rates in Patients Undergoing Open and Endovascular repair of Popliteal Artery Aneurysms
Karan Garg, MD, Caron B. Rockman, MD, Firas F. Mussa, MD, Thomas S. Maldonado, MD, Glenn R. Jacobowitz, MD, Todd L. Berland, MD, Mark A. Adelman, MD, Frank J. Veith, MD, Neal S. Cayne, MD.
NYU Langone Medical Center, New York, NY, USA.
Objective: Endovascular repair (ER) of popliteal artery aneurysms (PAA) has emerged as a minimally invasive alternative to open repair (OR). This study compares patency rates in those undergoing ER and OR of PAAs.
Methods: A retrospective chart review was performed to identify PAAs repaired between 1998 and 2012. Graft patency was based on either clinical (presence of palpable pulses) and/or radiologic examination.
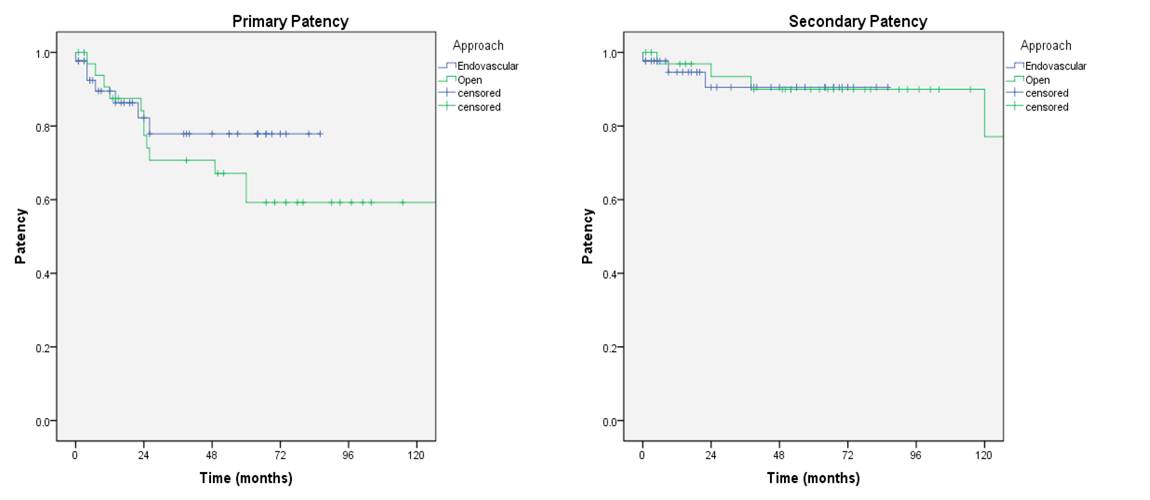
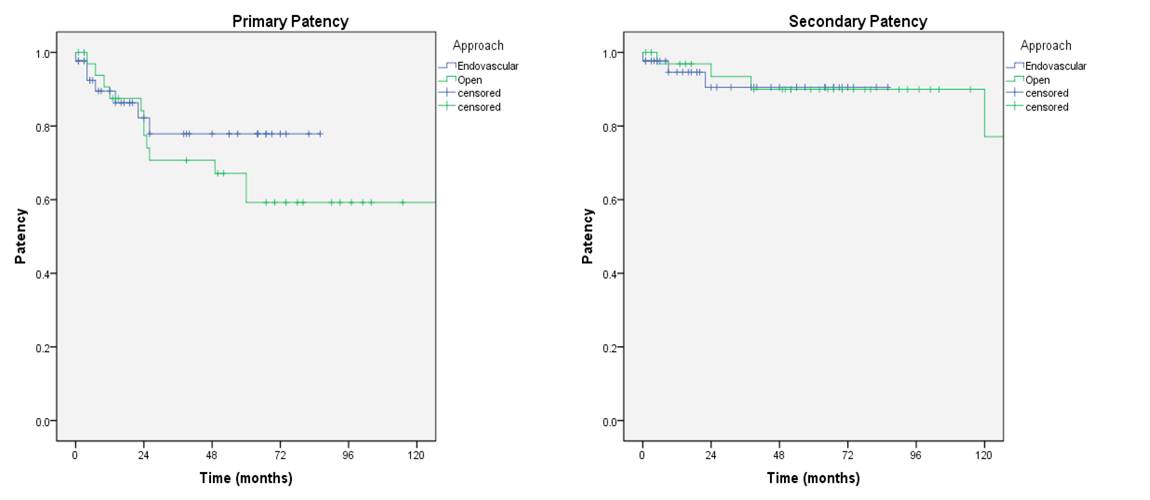
Results: A total of 69 patients with 79 PAAs underwent repair. Thirty-two patient (36 limbs) underwent OR while 38 patients (43 limbs) underwent ER. All ERs utilized the Viabahn endoprosthesis (W.L. Gore, Flagstaff, AZ), while ORs were utilized autologous great saphenous vein or prosthetic grafts. Postoperative treatment consisted of antiplatelet therapy, anticoagulation or both. The patient cohorts were similar at baseline between the OR and ER groups (p>0.05) - mean age 70.6 ± 13.1 versus 74.5 ± 9.0 years; mean diameter of 3.21 ± 1.54 cm versus 2.77 ± 0.88 cm; mean runoff of 2.06 ± 0.80 versus 2.0 ± 0.76 vessels; and symptomatic aneurysms in 41.7% versus 30.2% of cases. 55.8% of cases were performed under loco-regional anesthesia in the ER group, compared to 44.4% in the OR group. Length of stay was significantly shorter in the ER group, 1.95 ± 2.05 versus 6.38 ± 5.05 days in the OR cohort (p<0.001). Mean follow up was significantly longer in the OR group, 75.3 ± 68.5 months versus 33.8 ± 27.3 months (p0.05). The secondary patency improved to 90% and 90.5% (Figure 1). One patient undergoing OR required an amputation. Single vessel runoff was associated with higher occlusion rates among all patients undergoing repair (p=0.004) and the ER cohort (p=0.003), but not the OR group. Furthermore, patients with good run-off (two or three vessels) undergoing ER had fewer instances of graft occlusion, 3.1% versus 24% (p=0.036).
Conclusion: Patients undergoing OR had a decreased primary patency, however, close surveillance and prompt reinterventions resulted in secondary patency comparable to ER. Patients with good run-off had improved primary patency with ER.
Back to Annual Symposium Program

|