|
Back to 2015 Annual Symposium Program
Improved Access to Healthcare in Massachusetts after 2006 Massachusetts Healthcare Reform is Associated with a Significant Decrease in Mortality among Vascular Surgery Patients
Mohammad H. Eslami, MD1, Denis V. Rybin, MS2, Gheorghe Doros, PhD2, Alik Farber, MD1.
1Division of Vascular and Endovascular Surgery, Boston University School of Medicine, Boston, MA, USA, 2Department of Biostatistics, Boston University School of Public Health, Boston, MA, USA.
Introduction: Timely access to care is directly impacted by insurance coverage and affects outcomes after vascular procedures. We evaluated trends of in-hospital mortality (IHM) for index vascular procedures so as to assess the effects of 2006 Massachusetts (MA) Healthcare Reform (MHR) on the mortality trends.
Methods: National Inpatient Sample (2003-2011) was queried to identify surgical patients with peripheral arterial disease, carotid stenosis and abdominal aorta aneurysm based on ICD-9CM diagnostic and procedure codes. The cohort was then divided into MA and non-MA (NMA) based on the location of the hospital. Two time intervals, 2003-2006 (P1) and after 2006 (P2) were selected for comparisons. The patients at MA and NMA hospitals were described in terms of demographic characteristics and presentation by time interval (P1 vs. P2) and compared using Chi-Square and T-test. Weighted logistic regression with a term modeling change in the odds ratio (OR) for second time interval was used to test and estimate trends in mortality and to compare MA and NMA trends.
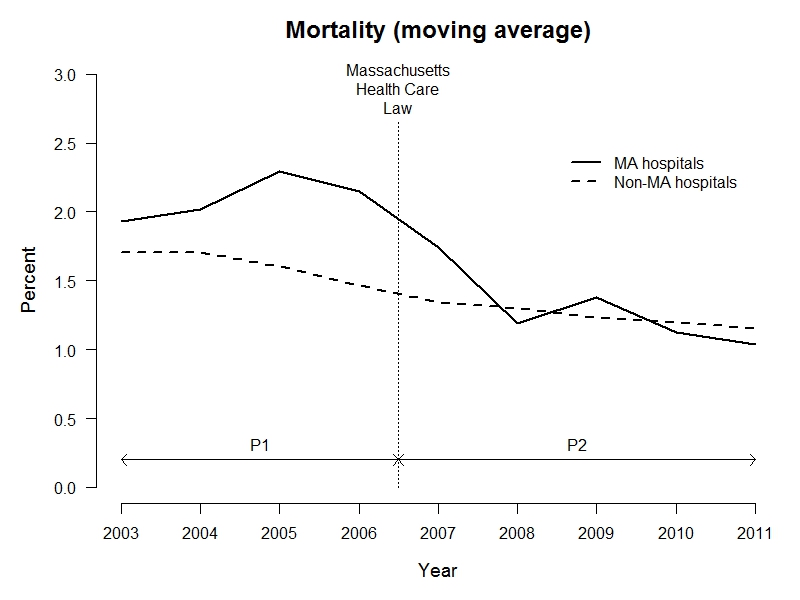
Results: We identified 306,438 patients operated on for PAD, CS and AAA. MA and NMA cohorts were similar with a significant increase in Elixhauser comorbidity index in P2 (vs. P1) in both cohorts (p<0.001). Mortality trends are depicted in Figure 1. There was a significant decline in IHM for all vascular patients during both time intervals, although no significant difference in the rate of decline was noted (Table). There was no significant difference in IHM trends in P1 between MA and NMA; however, a significantly higher decrease in IHM was noted in MA compared to NMA in P2 (the annual odds ratio of IHM differ by 18%, p=0.010).
Conclusions: Overall a significant decrease in IHM for all vascular procedures was noted in the US. The decline in postoperative IHM was significantly more rapid in MA after 2006 compared to NMA sample. This study suggests that better access to care in MA may be a cause of this decline in IHM.
Annual change in In-hospital Mortality after Vascular Operations| Contrast | Odds Ratio | 95% Confidence Interval | p Value | Overall Annual Change:
2003-2006 (P1)
2007-2011 (P2)
P2 vs. P1 | 0.93
0.95
1.02 | 0.90, 0.97
0.93, 0.97
0.96, 1.08 | <0.001
<0.001
0.569 | MA Annual Change:
P1
P2
P2 vs. P1 | 1.05
0.78
0.74 | 0.85, 1.29
0.67, 0.91
0.56, 0.99 | 0.648
0.001
0.043 | Non-MA Annual Change:
P1
P2
P2 vs. PA | 0.93
0.95
1.03 | 0.90, 0.97
0.93, 0.98
0.97. 1.09 | <0.001
<0.001
0.405 | MA vs. Non-MA (P1)
MA vs. Non-MA (P2) | 1.13
0.82 | 0.92, 1.39
0.70, 0.95 | 0.260
0.010 | 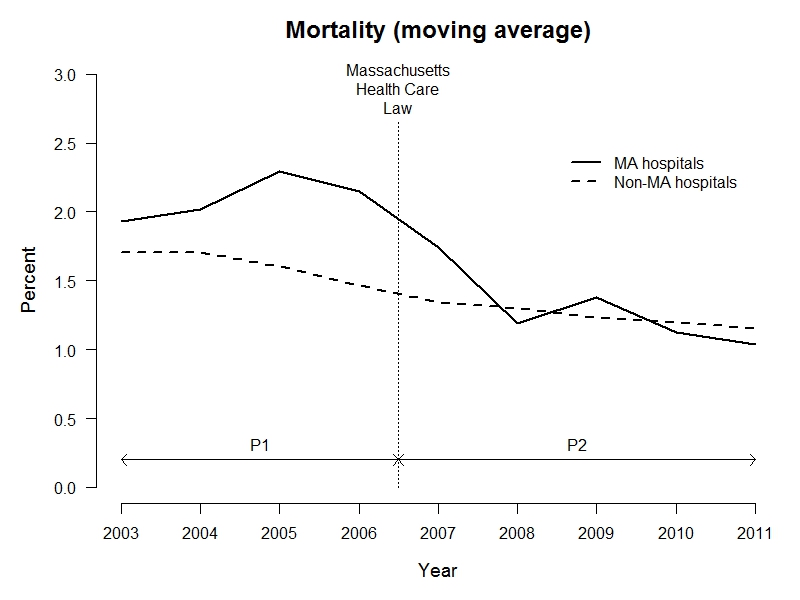
Back to 2015 Annual Symposium Program
|