|
Back to 2015 Annual Symposium Program
Clinical Results of Single versus Multiple-Vessel Infrapopliteal Intervention
Jeremy D. Darling, B.A., John C. McCallum, M.D., John Hon, B.S., Sara L. Zettervall, M.D, Peter Soden, M.D., Dominique B. Buck, M.D, Raul Guzman, M.D., Marc L. Schermerhorn, M.D.
Beth Israel Deaconess Medical Center, Boston, MA, USA.
OBJECTIVES:
The effects of concomitant endovascular interventions on multiple infrapopliteal vessels are not well known and the long-term sequelae of such procedures have not been reported.
METHODS:
From 2004 to 2014, 673 patients underwent an infrapopliteal endovascular intervention for tissue loss (77%), rest pain (13%), stenosis of a previously treated vessel (5%), acute limb ischemia (3%), or claudication (2%). Data collected included RAS events (revascularization, major amputation, or stenosis [>3.5x step-up by duplex]) and wound healing. Patients without an initial indication of Critical Limb Ischemia (CLI) were excluded. Patients were characterized by single-vessel infrapopliteal interventions and multiple-vessel infrapopliteal interventions. Worsened Rutherford class between index procedure and failure was also noted.
RESULTS:
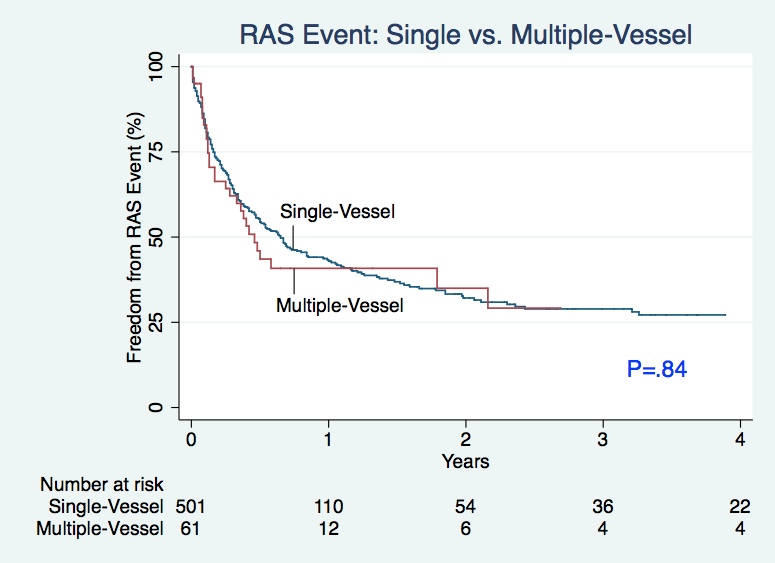
Of the 673 patients, 596 underwent an infrapopliteal endovascular intervention for CLI: 85% for tissue loss and 15% for rest pain. During a single procedure, 533 (89%) patients underwent a single-vessel intervention while 63 (11%) patients underwent a multiple-vessel intervention. Patients undergoing a single-vessel intervention had more commonly experienced a prior ipsilateral endovascular procedure (17% vs. 10%, P=.04) while patients undergoing a multiple-vessel intervention more often suffered from diabetes (78% vs. 89%, P=.03) and were more often discharged to a rehab facility (33% vs. 41%, P=.04). Survival analysis revealed no difference in the proportion of patients experiencing a restenosis (P=.11). A Cox regression model illustrated that long-term outcomes do not differ between patients undergoing a multiple-vessel intervention versus those undergoing a single-vessel intervention. Among the 596 patients, a RAS event occurred in 284 limbs (48%) and there was no significant difference in the rate of RAS events between single and multiple-vessel infrapopliteal interventions (48% vs. 49%, p=.84). Amputation rate also did not significantly differ between the two groups (14% vs. 16%, P=.71). In both groups, 8% of RAS patients presented with a worse ischemia class as compared to their initial symptoms.
CONCLUSIONS:
Our data suggest that multiple-vessel intervention does not improve outcomes as compared to single-vessel intervention following any infrapopliteal procedure for CLI. 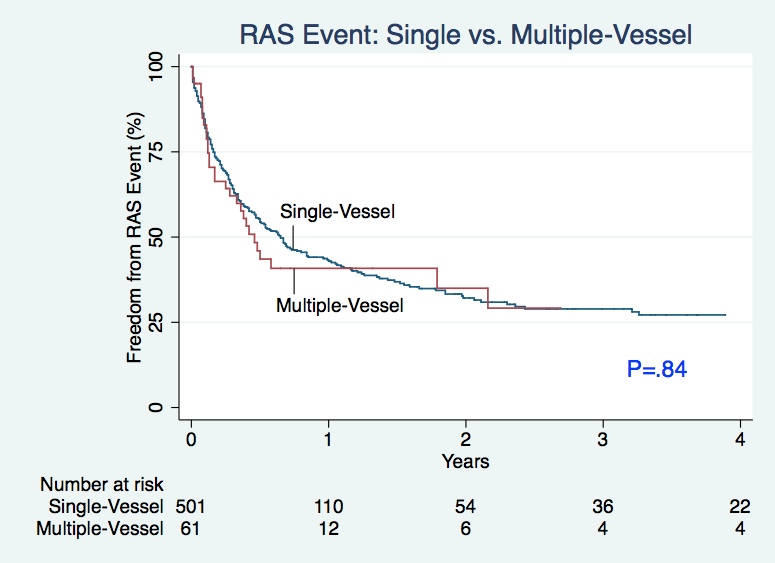
Back to 2015 Annual Symposium Program
|