Back to 2015 Annual Symposium Program
External Validation of Vascular Group of New England (VSGNE) Risk Predictive Model of Mortality after Elective Abdominal Aorta Aneurysm Repair (EAR) and Comparison against Established Models.
Mohammad H. Eslami, MD1, Denis Rybin, MS2, Gheorghe Doros, PhD2, Alik Farber, MD1.
1Division of Vascular and Endovascular Surgery, Boston University School of Medicine, Boston, MA, USA, 2Department of Biostatistics, Boston University School of Public Health, Boston, MA, USA.
Introduction: Previously, we developed a VSGNE risk predictive model (RPM) to predict in-hospital mortality (IHM) after EAR. The purpose of this study is to externally validate this model using American College of Surgeons’ National Surgical Quality Improvement Program (NSQIP) database and evaluates its ability to predict mortality compared to established RPMs.
Methods: VSGNE AAA database was queried for patients who underwent EAR. Only pre-operative variables, Anesthesia Society Association (ASA) classification and type of procedure were entered into a logistic regression model as predictors of IHM. Backward elimination procedure with alpha level of 0.2 was used to select a more parsimonious model. Calibration was performed to measure how closely predicted outcomes agree with observed outcomes. The predictive value of the model was assessed via C-statistic. Hosmer-Lemeshow (HL) method was used to assess calibration. The external validation of this model was performed using the NSQIP EAR sample. This model was then compared to Medicare (MED) and Glasgow Aneurysm Score (GAS) for predicting IHM in NSQIP sample. Vuong test was performed to compare model fit. Model discrimination was assessed in equally-sized risk-group NSQIP terciles.
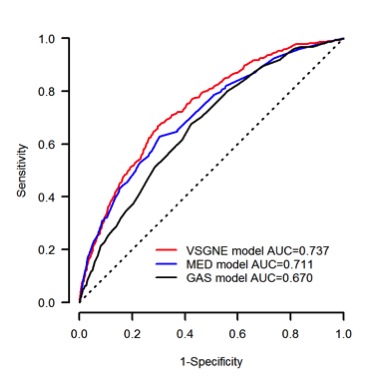
Results: Data from 2,681 patients from the VSGNE sample with overall 1.3% IHM rate were used to develop a parsimonious AAA mortality model (Table). Internally validated model showed a very high discriminating ability (Corrected C= 0.805) and good model fit (HL p=0.699). External validation on 18,766 NSQIP patients with an overall 1.9% IHM rate showed very good predictive ability (AUC=0.737, Fig). Vuong tests yielded a significant fit difference favoring MED and VSGNE to GAS model while MED and VSGNE compared similarly (Fig). Across three risk terciles, VSGNE model predicted observed mortality reasonably well.
Conclusion: The VSGNE AAA RPM was externally validated on NSQIP AAA patients and shows a high fidelity for predicting EAR mortality performed by a diverse array of physicians. A risk score based on this model can reliably stratify patients according to their risk of mortality after EAR.
AAA Final Risk Predictive Model of Mortality| Variable | Beta | Standard Error | p Value | | Intercept | -12.54 | 2.17 | <0.001 | | Open Procedure | 1.35 | 0.37 | <0.001 | | Age | 0.09 | 0.03 | 0.001 | | Female Gender | 0.88 | 0.36 | 0.014 | | Myocardial Disease | 0.62 | 0.36 | 0.088 | | Vascular Disease | 0.80 | 0.42 | 0.060 | | Congestive Heart Failure | 0.88 | 0.41 | 0.032 | | Chronic Obstructive Pulmonary Disease | 0.55 | 0.36 | 0.126 | | ASA: Life Threat/Moribund | 0.90 | 0.80 | 0.260 | 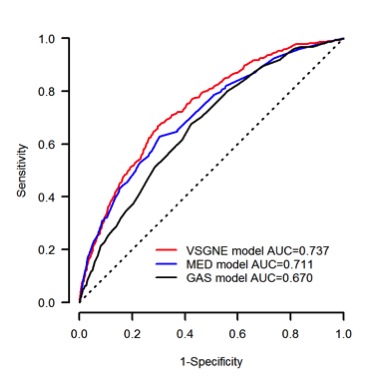
Back to 2015 Annual Symposium Program
|