|
Back to 2015 Annual Symposium Program
Predictive Ability of the SVS Lower Extremity Guidelines Committee Wound, Ischemia, and foot Infection (WIfI) Scale
Jeremy D. Darling, B.A., John C. McCallum, M.D., Yifan Meng, B.S., Peter Soden, M.D., Sara Zettervall, M.D., Dominique Buck, M.D., Mark Wyers, M.D., Allen Hamdan, M.D., Marc L. Schermerhorn, M.D.
Beth Israel Deaconess Medical Center, Boston, MA, USA.
OBJECTIVES:
The Society for Vascular Surgery (SVS) Lower Extremity Guidelines Committee has composed a new threatened lower extremity classification system that reflects the three major factors that impact amputation risk and clinical management: Wound, Ischemia, and foot Infection (WIfI). Our goal was to evaluate the predictive ability of this scale following any infrapopliteal endovascular intervention for Critical Limb Ischemia (CLI).
METHODS:
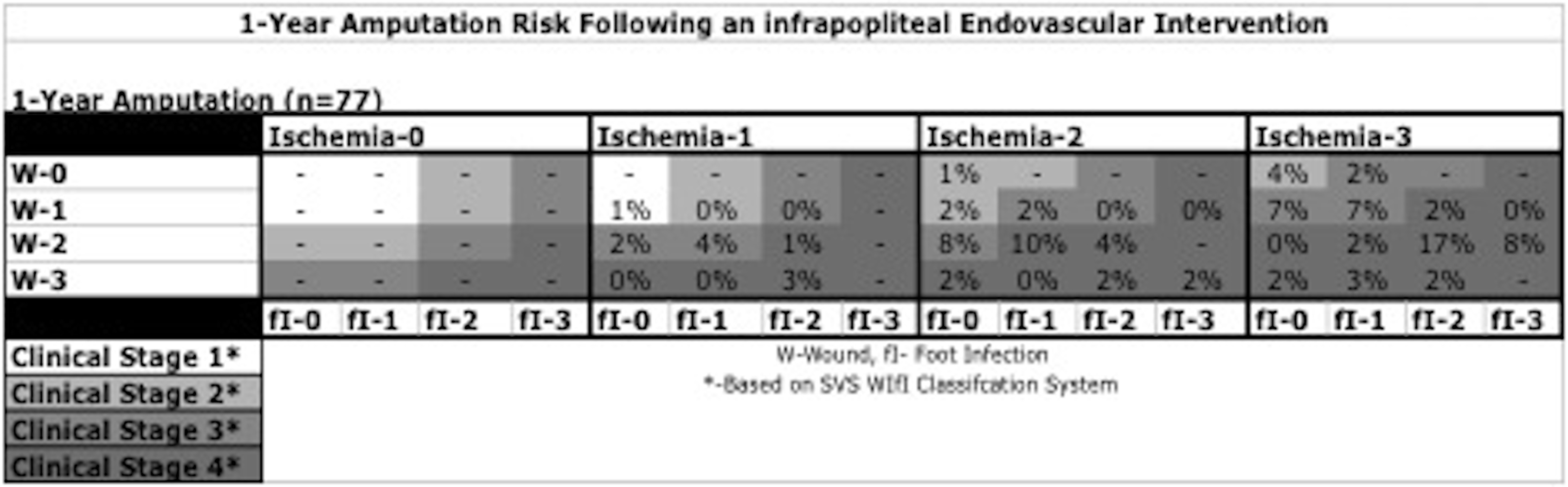
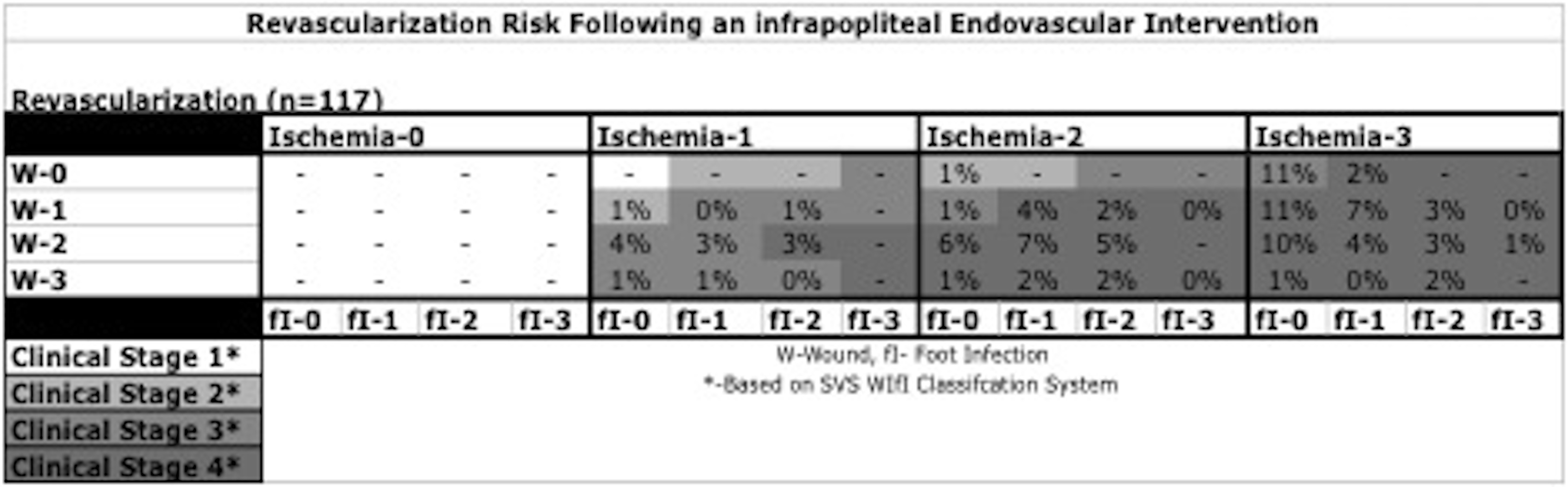
From 2004 to 2014, 673 patients underwent an infrapopliteal endovascular intervention for tissue loss (77%), rest pain (13%), stenosis of a previously treated vessel (5%), acute limb ischemia (3%), or claudication (2%). Patients without an initial grade in all WIfI categories were excluded. Patients were stratified both into clinical stages 1 to 4 based on the SVS WIfI classification for 1-year amputation and revascularization risk, as well as a novel composite score from 0 to 9. Outcomes included the SVS objective performance goals (major amputation, amputation-free survival, and wound healing) as well as mortality and RAS events (revascularization, major amputation, or stenosis [>3.5x step-up by duplex]). Analyses were performed using multivariable logistic regression, Cox regression models, and Kaplan-Meier survival estimates.
RESULTS:
Of the 596 CLI patients, 551 were classified in all three WIfI domains on a scale of 0 (least severe) to 3 (most severe). Of these 551 patients, 84% were treated for tissue loss and 16% for rest pain. A Cox regression model illustrated that an increase of 1 clinical stage increases the rate of major amputation (Hazard Ratio [HR], 1.4; 95% Confidence Interval [CI], 1.0-2.0). A separate regression model showed that a 1-unit increase in the composite WIfI scale is associated with an increase in the rate of RAS events (HR, 1.2; 95% CI, 1.1-1.3) and a decrease in wound healing (HR, 1.2; 95% CI, 1.0-1.3).
CONCLUSIONS:
This study suggests that the SVS WIfI classification system can predict 1-year amputation, RAS events, and wound healing following any endovascular infrapopliteal intervention for CLI. 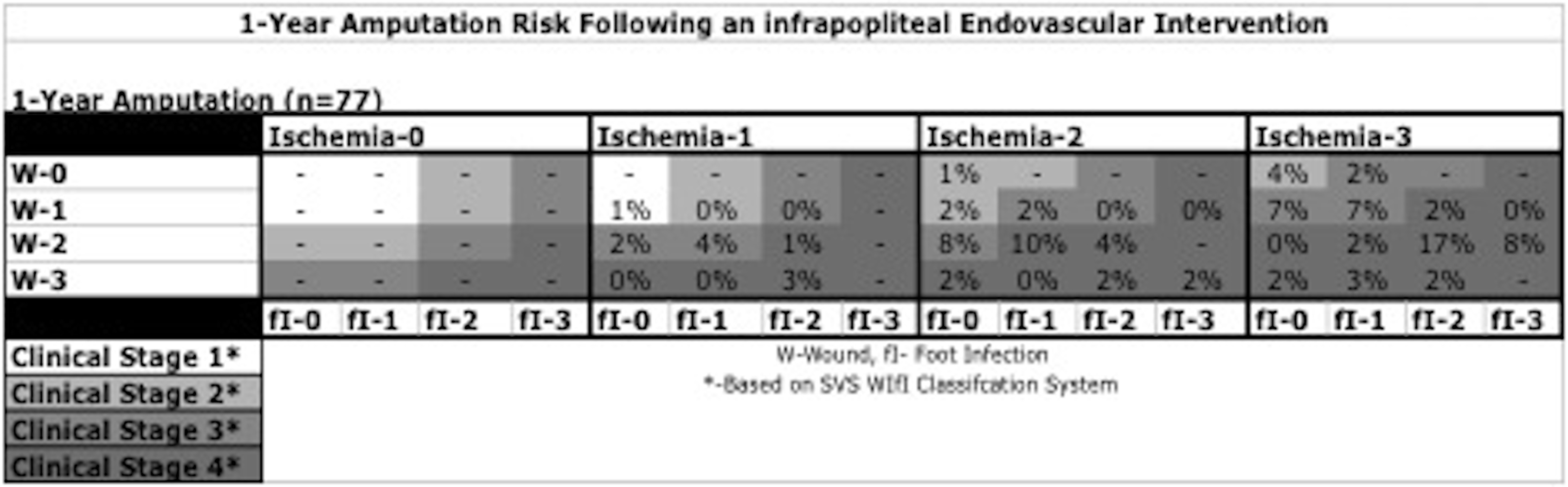 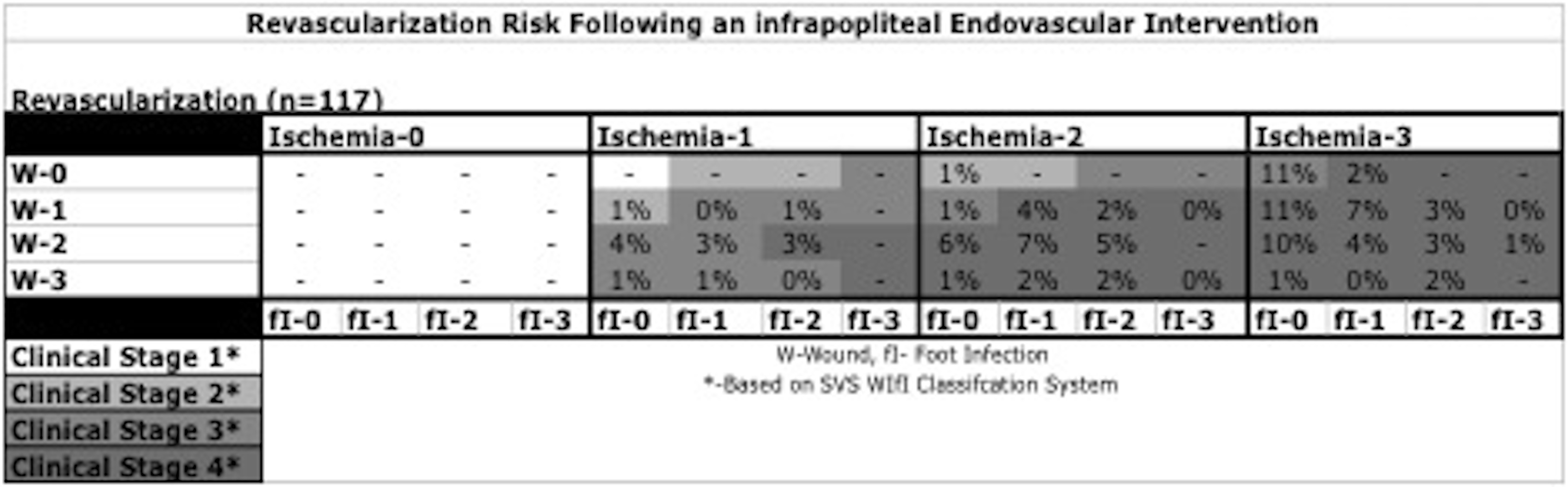
Back to 2015 Annual Symposium Program
|