|
Back to 2015 Annual Symposium Program
Different patterns of arterial occlusive disease in chronic critical limb ischemia between Blacks, Hispanics and Caucasians
Jayer Chung, MD, J Gregory Modrall, MD, Martyn Knowles, MD, Lawrence A. Lavery, DPM, MPH, Carlos H. Timaran, MD, R James Valentine, MD.
University of Texas Southwestern Medical Center, Dallas, TX, USA.
Objective: Quantify associations between ethnicity and anatomic patterns of arterial occlusive disease in chronic critical limb ischemia (CLI), adjusting for known co-variates.
Methods: Retrospective review of a prospective database of consecutive CLI patients presenting to the vascular surgery service. Computed tomographic angiograms (CTAs) and digital subtraction angiograms (DSAs) were reviewed. Arterial lesions were defined by location (Aortoiliac=aorta and iliac arteries; Femoral=common, profunda, and superficial femoral arteries; and Popliteal-tibial=infrapopliteal and tibial arteries). Stenoses > 50% were deemed hemodynamically significant. Associations between the arteriographic patterns of disease, baseline demographics and medical co-morbidities were quantified using Kruskal-Wallis, χ2, and Maentel-Haenszel χ2 tests.
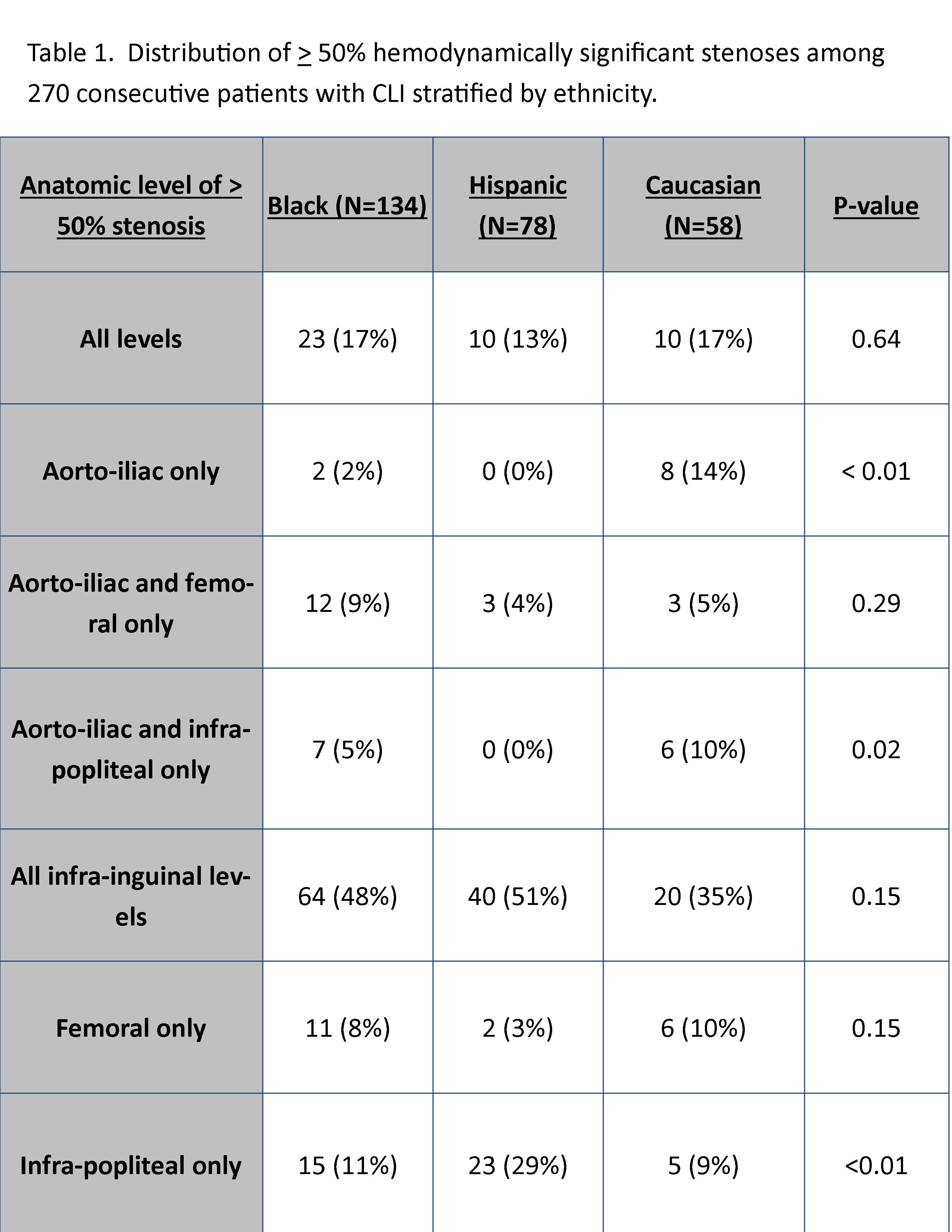
Results: Between August 2010 and January 2014, 286 patients (N=172 male, N=143 with tissue loss) presented. 270 subjects had arteriograms (Black N=134, 50%; Hispanic N=78, 29%; Caucasian N=58, 21%; Table 1.) Hispanics (N=23, 30%) presented with the highest incidence of isolated infra-popliteal disease (IPD; p=0.02, χ2). Caucasians (N=8, 14%) presented more frequently with aorto-iliac occlusive disease than either Hispanics or Blacks (p < 0.01,χ2 ). Diabetes mellitus was more prevalent in Hispanics (N=72, 85%) relative to Blacks (N=77, 55%) and Caucasians (N=32, 52%; p < 0.001,χ2 ). Median Hemoglobin A1c (HbA1c) was also higher among Hispanics (7.3%, IQR 6.2, 9.9) versus Blacks (6.6%, IQR 5.8,8.2) and Caucasians (6.0%, IQR 5.6,7.6; p=0.002, Kruskal-Wallis). More Caucasians (N=53, 87%) and Blacks (N=113, 81%) abused tobacco compared to Hispanics (N=48, 57%; p=0.001, χ2.) When stratified by baseline HbA1c, there was no relationship between ethnicity and IPD with HbA1c 8.9% had a significantly higher probability of having IPD (p=0.005, Maentel-Haenszel χ2). Smoking was not associated with any anatomic pattern of disease (p = NS, Maentel-Haenszel χ2.) Use of statin, anti-platelet, beta-blocker, angiotensin-converting enzyme inhibitor/angiotensin-receptor blocking medications was similar across all ethnicities (p=NS, χ2).
Conclusions: Hispanic patients present more frequently with IPD, which may contribute to previously reported outcome disparities. IPD may be modifiable, as the most severely afflicted diabetics are at the highest risk. Future interventions to improve outcomes should aim to understand mechanisms of diabetic arteriopathy and barriers to proper glycemic control, especially among Hispanics. 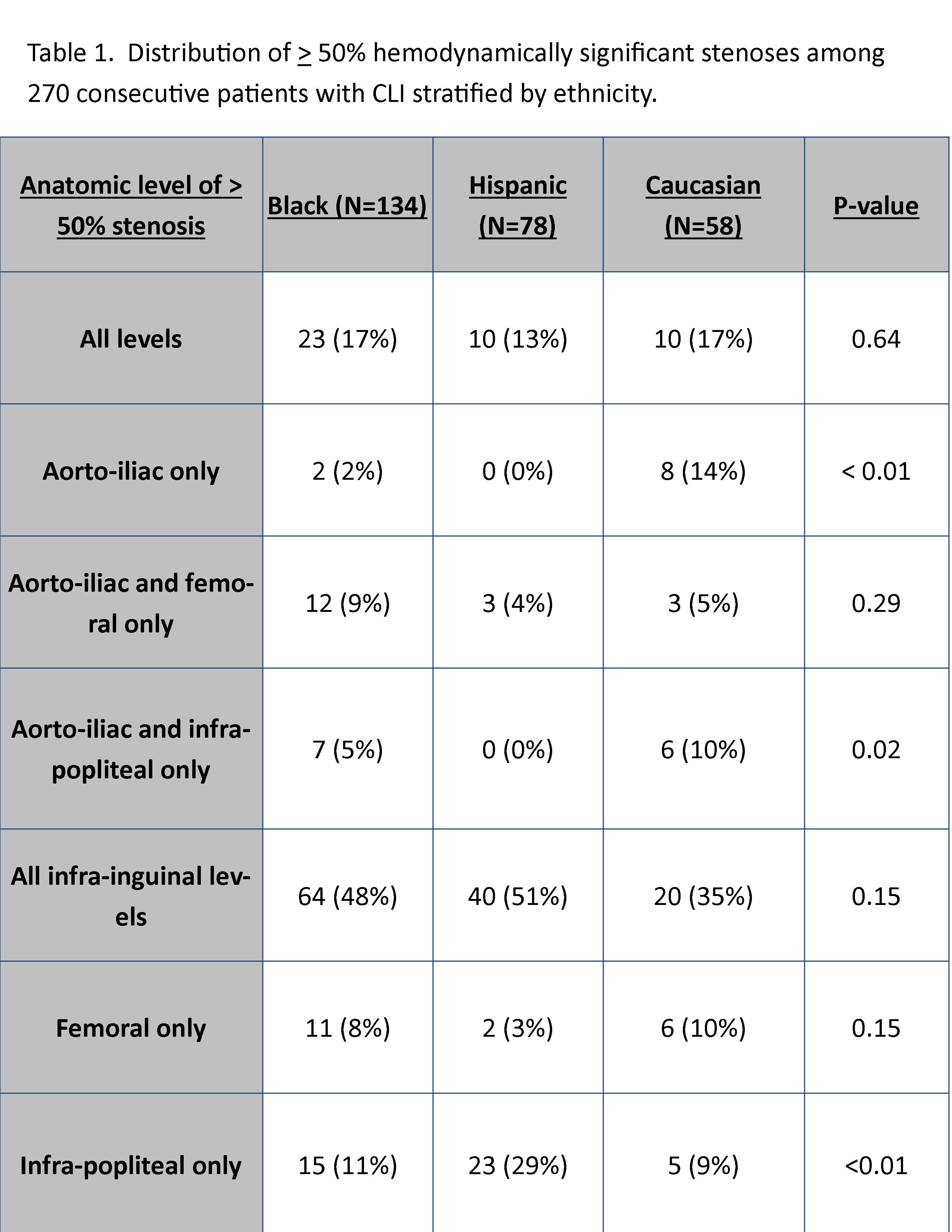
Back to 2015 Annual Symposium Program
|