Back to 2015 Annual Symposium Program
Predictors of Mortality in Abdominal Aortic Aneurysm Repair for Nonagenarians: Analysis of the NSQIP Dataset
Jimmi Mangla, MD, Christina Jenkins, MD, Mohsen Bannazahdeh, MD, Elizabeth Gates, RN, Graham W. Long, MD, O W. Brown.
William Beaumont Hospital, Royal oak, MI, USA.
Objective: Increased longevity and incidental detection of abdominal aortic aneurysms (AAA) on imaging for other causes have led to increased prevalence of clinically significant (> 4 cm) AAA in nonagenarians. Previous studies have reported outcomes of AAA repair in nonagenarians. However, these involved small cohorts and factors contributing to mortality were not quantified. Our objective was to analyze predictors of mortality among nonagenarians undergoing endovascular aortic aneurysm repair (EVAR) and open surgical repair (OSR).
Methods: Nonagenarians who underwent AAA repair between January 2005 and December 2012 were identified using the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) participant use data files. Multivariate step-down logistic regression was used to identify predictors of 30-day mortality.
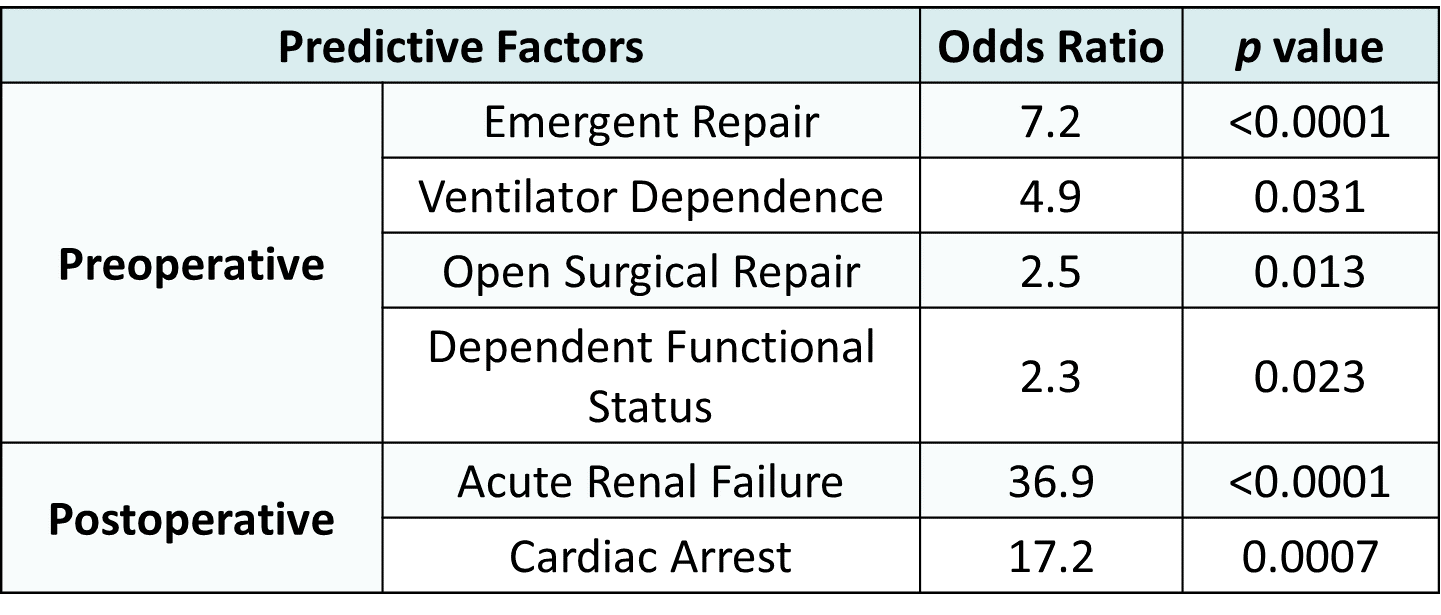
Results: Of 642 nonagenarians who underwent AAA repair, 552 (86%) had EVAR and 90 (14%) had OSR. Eighty-three patients underwent emergent EVAR and fifty-five patients had emergent OSR. Overall 30-day mortality was 7.3% in EVAR versus 38.9% in OSR (Odds Ratio (OR) 8.15, p<0.0001). Mortality in patients undergoing elective EVAR was significantly less than in those undergoing elective OSR (3.2% versus 16.1%, p=0.01). Similarly, mortality in patients undergoing emergent EVAR was significantly less than those with emergent OSR. (31.6% versus 50.8%, p=0.03). Preoperative predictive factors for 30-day mortality in a multivariate step-down logistic regression model (Table) included ventilator dependence, dependent functional status, OSR, and emergent repair. Postoperative acute renal failure and cardiac arrest were also predictive of 30-day mortality. This predictive model has a c-statistic of 0.88, indicating a strong association of predicted probabilities with observed outcomes.
Conclusions: Elective EVAR is associated with an acceptably low 30-day mortality rate in nonagenarians. If technically feasible, EVAR should be first line surgical therapy in nonagenarians with AAA in both elective and emergent situations. Factors predictive of mortality can be utilized in perioperative risk stratification and during the informed consent process in these very elderly patients. 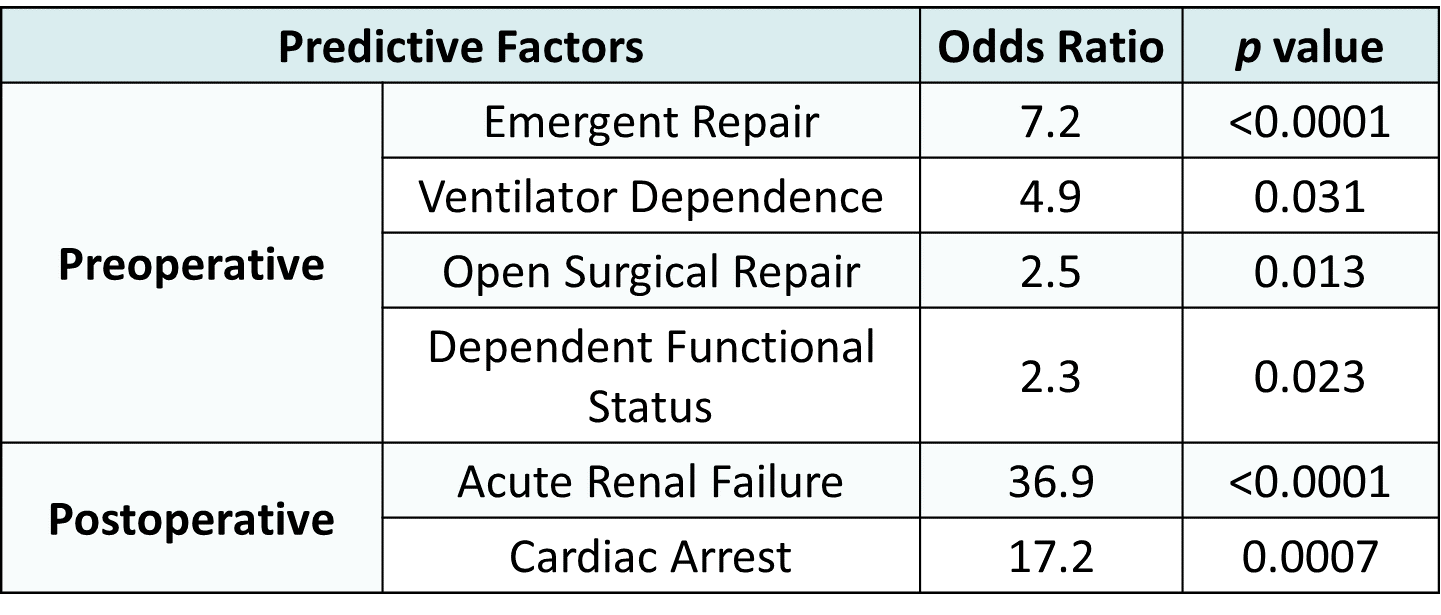
Back to 2015 Annual Symposium Program
|