Back to 2015 Annual Symposium Program
Long-Term Patency Of Primary Inferior Vena Cava Reconstructions
George E. Havelka, MD, Heron E. Rodriguez, MD, Andrew W. Hoel, MD, Mark K. Eskandari, MD.
Northwestern University, Chicgo, IL, USA.
Objective: Inferior vena cava (IVC) repair after planned and unplanned venotomy may take the form of either interposition bypass, patch venopasty or lateral venorrhaphy and primary repair. Direct repair of the IVC avoids the use of foreign material, and allows for an all-autologous repair in an expeditious fashion. Furthermore, primary repair can be accomplished without compromising venous outflow from the lower extremities and exhibits excellent long-term patency rates.
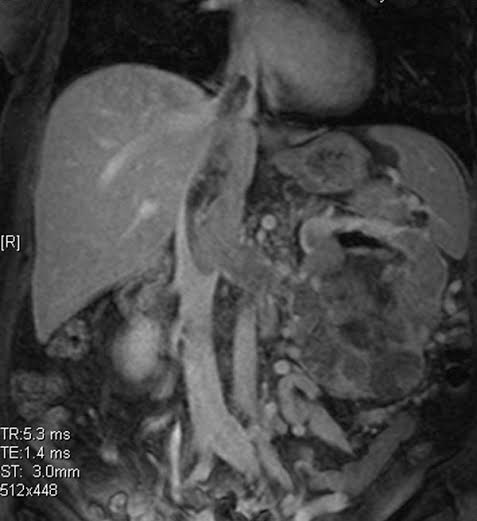
Methods: Enrollment consisted of 47 consecutive patients who underwent direct IVC repairs between January 2002 and January 2014. Primary repair followed lateral venorrhaphy for tumor extraction (figure 1) or to repair an iatrogenic or traumatic IVC injury. Patient demographics, vena cava dimensions and patient outcomes were tabulated.
Results: Most patients underwent en bloc nephrectomy, IVC tumor thrombus extraction and primary lateral venorrhaphy; 92% had RCC on final pathology. This group consisted of 15 men and 11 women; the average age was 61.0 years (39-83 years); the mean operative time was 410.3 ± 119.9 minutes; mean estimted blood loss (EBL) was 3395.4 mL and the mean follow-up period was 38.1 months (1-96 months). Complications included one pulmonary embolism and one case of anuria requiring re-operation. Five patients required a supra-hepatic IVC clamp associated with a longer operative time compared to those requiring an infrahepatic clamp (532 minutes vs. 360 minutes, respectively). The group undergoing primary repair for iatrogenic or penetrating traumatic IVC injury consisted of 15 men and 6 women; the average age was 52.7 years (31-82 years); the mean operative time was 366.1 ± 137.9 minutes; mean EBL was 1610.1 mL and the mean follow-up period was 20.2 months (3-92 months). Complications included one pleural effusion requiring chest tube drainage and one hospital acquired pneumonia. There were no intra-operative deaths nor pulmonary emboli in either group.
Neither group exhibited post-op clinical or radiographic evidence of IVC stenosis or occlusion.
Conclusion: Regardless of the indication or the level of IVC clamping, primary IVC repair is a safe, expeditious technique that provides good long-term patency.
2 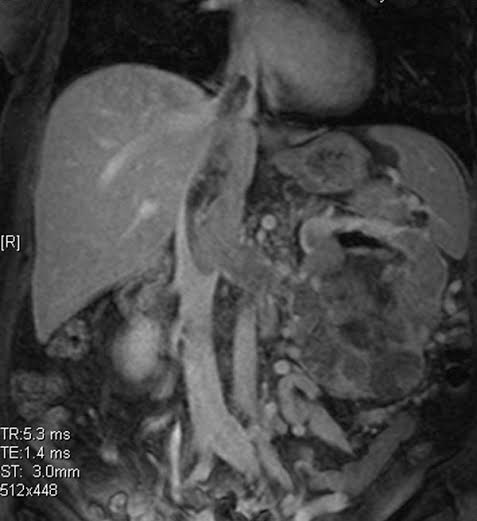
Back to 2015 Annual Symposium Program
|