|
Back to 2015 Annual Symposium Program
Contemporary outcomes of open and endovascular popliteal artery aneurysm repair
Andrew E. Leake, MD, Rabih Chaer, MD, Michael Singh, MD, Michel Makaroun, MD, Luke Marone, MD.
UPMC, Pittsburgh, PA, USA.
Introduction:
The purpose of this study was to evaluate contemporary results and outcomes of open repair (OR) or endovascular repair (ER) for popliteal artery aneurysms (PAA).
Methods:
Consecutive patients with PAA treated from January 2006 to March 2014 were reviewed under an IRB approved protocol. Demographics, anatomic characteristics, and outcomes were collected. Most acute cases were managed by OR with an increasing trend of ER use in elective procedures, all treated with Viabahn stent grafts (WL Gore, Flagstaff, AZ). Standard statistical methods were used.
Results:
186 PAAs were repaired in 156 patients (110 OR, 76 ER). Mean age was 71 years and most were male (96%). Mean follow up was 32.3 months (OR 34.8, ER 28.3, P=NS). Co-morbidities were similar between groups. Concomitant aneurysms were noted in the common femoral artery (10%) and the abdominal aorta (47%). OR included more patients with PAA thrombosis (41.8% vs. 5.3%, P<.001), acute ischemia (24.5% vs. 9.2%, P=.01) and ischemic rest pain (34.5% vs. 6.6%, P<.001). Mean tibial runoff score was 5 for OR vs. 3.3 for ER (P=.006).
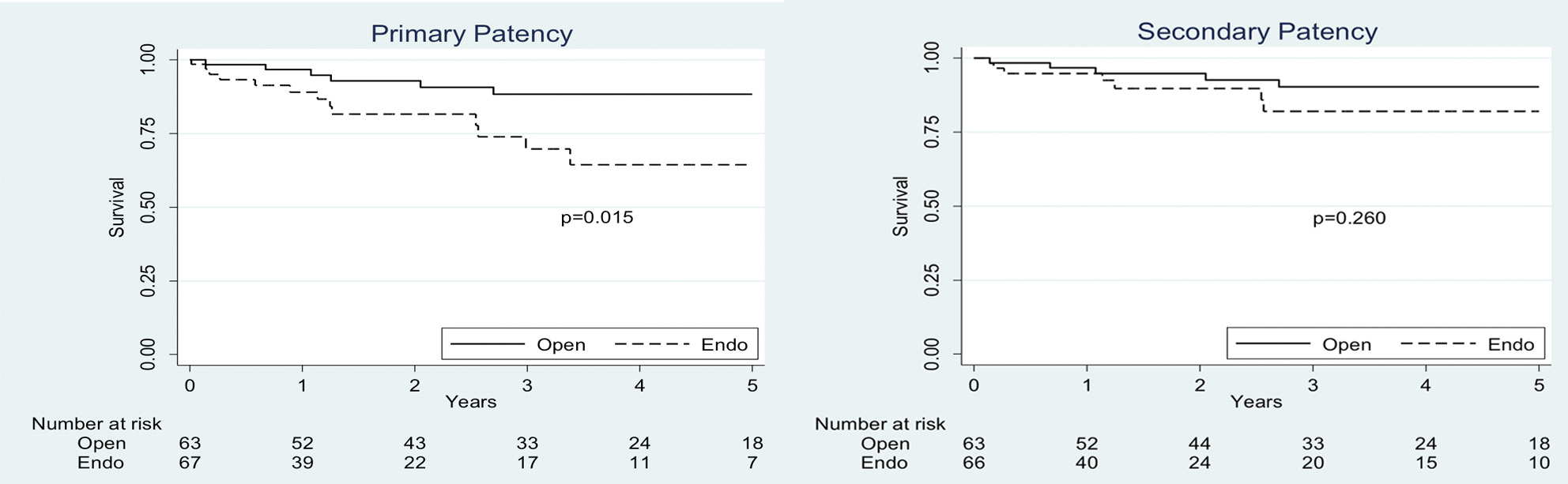
OR had increased 30-day complications (22% vs. 2.6%, P<.001), and mean length of stay (5.8d vs. 1.6d, P<.001). OR complications were related to infections (10%), bleeding (5%), or thrombosis (2%). Mortality was slightly higher in OR (1.8% vs 0%, p=NS) as was major amputation rate (3.7% vs1.3%, P=NS). Primary, primary-assisted and secondary patency rates were similar to 3 years (OR: 79.5, 83.7 and 85% vs ER: 73.2, 76.3 and 83% p=NS). ER thrombosis was noted in 8/24 patients treated in 2006-08 (33% @ mean 19.6m), but only 4 of 51 in 2009-13 (7.8% @ mean 12m), suggesting a steep learning curve.
Among 130 patients presenting electively without acute ischemia or thrombosed PAA (63 OR and 67 ER), OR had better 3 year primary (88.3 vs 69.8, p=.03) and primary assisted (90.2 vs 73.5% p=.051) but similar secondary patency (90.2 vs 82% p=.26). (Figure).
Conclusion:
Endovascular repair is a safe and durable option for PAA repair, with lower complications and shorter length of stay. Notwithstanding, open repair appears to have superior durability in elective patients. 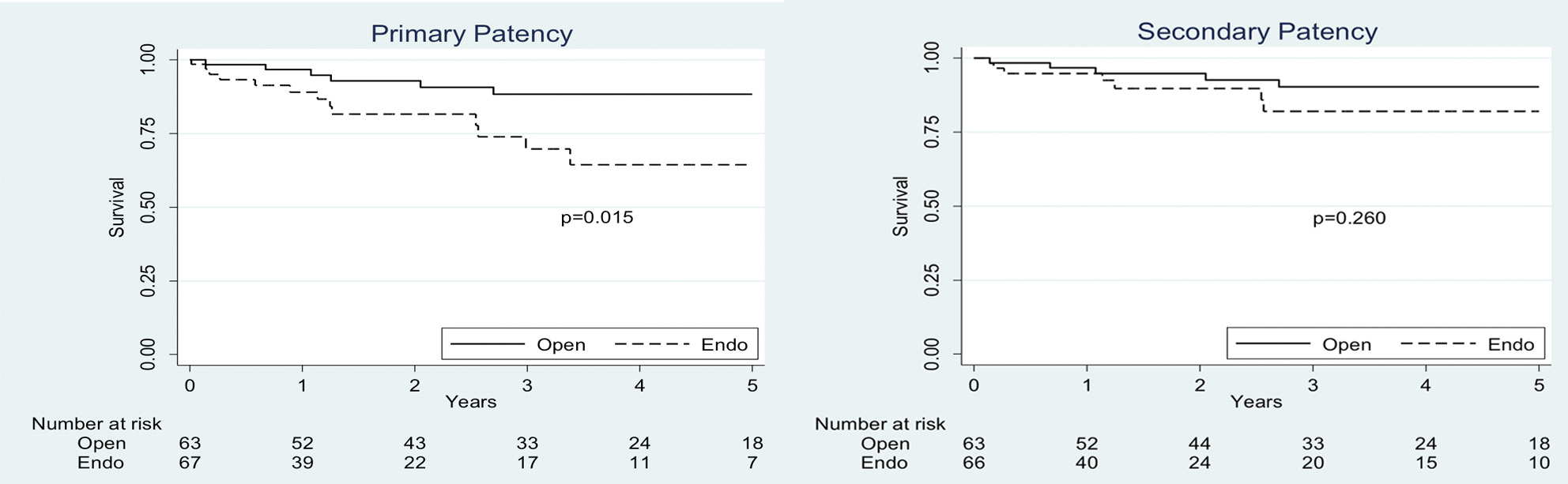
Back to 2015 Annual Symposium Program
|