Back to 2016 Annual Symposium Abstacts
Minimizing Interval between Revascularization and Completion Amputation Optimizes Surgical Site Healing
Brett C. Chatman, DPM, Caitlin M. Sorensen, BA, MS, Matthew E. Snow, DPM, Michael C. Siah, MD, Katherine M. Raspovic, DPM, Tareq M. Massimi, MD, Edward Y. Woo, MD, Steven D. Abramowitz, MD.
MedStar Washington Hospital Center, Washington, DC, USA.
Introduction:
Revascularization for patients presenting with wounds related to peripheral vascular disease (PVD) is integral to effective limb salvage techniques. Current literature does not delineate defined intervals between revascularization and definitive surgical intervention. This study incorporates a multidisciplinary approach between vascular surgery and podiatric surgery to determine if decreased time between revascularization and completions amputation leads to shorter healing time and improved limb salvage rates.
Methods:
This study is based upon a prospectively maintained retrospective single-center database from 2013-2015. Patients presenting with CLI were evaluated by an interdisciplinary team of vascular and podiatric surgery. Risk stratification using the WIFI classification system separated patients into low risk (class 1-2) and high risk (class 3-4) cohorts. Inclusion criteria consisted of patients initially staged at a WIFI class 3 or 4 who underwent endovascular revascularization followed by early podiatric surgical intervention. Follow-up appointments were reviewed and healing times were recorded. Statistical analysis was performed using non-parametric Spearman Correlation.
Results:
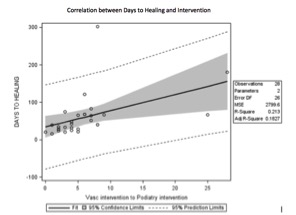
485 patients with CLI in the study period were identified. Of these patients, 30 were classified as WIFI class 3 or 4, and had complete records throughout the studied follow up period. Patients with 8 or less days between vascular and podiatric intervention were associated with greater than 34% reduction in time to healing, with average surgical site healing time of 17.9 days. Statistical analysis showed a positive correlation between decreased days to healing and reduced interval between revascularization and completion amputation. (r=0.68, p < 0.0001). For every one day decrease between vascular intervention to podiatric intervention, days to healing reduced by 4.33 days on average (p = 0.0134).
Conclusions:
In our system, a coordinated multidisciplinary approach to patients presenting with PVD and lower extremity wounds improved time to healing in patients with a high risk for a major amputation. This suggests that decreased time between revascularization and definitive surgical intervention significantly optimizes wound healing.
Back to 2016 Annual Symposium Abstacts
|