|
Back to 2016 Annual Symposium Abstacts
Predicting Neurologic Complications and 30-day Mortality after Thoracic Endovascular Aortic Repair in the Vascular Quality Initiative
Salvatore T. Scali, M.D., Robert J. Feezor, M.D., Dan Neal, M.S., Kristina A. Giles, M.D., Javairiah Fatima, M.D., Scott A. Berceli, M.D., Ph.D., Thomas S. Huber, M.D., Ph.D., Adam W. Beck, M.D..
University of Florida-Gainesville, Gainesville, FL, USA.
OBJECTIVES: Thoracic endovascular aortic repair (TEVAR) is a complex operation that has significant risk of neurologic morbidity and mortality. We sought to analyze the Vascular Quality Initiative (VQI) to determine rates of spinal cord ischemia (SCI), stroke, and 30-day mortality after TEVAR and identify preoperative predictors of these outcomes.
METHODS: All TEVAR procedures(2013-2014) in the VQI were reviewed. Incident rates of in-hospital SCI, stroke and 30-day mortality were captured. A composite end-point of any stroke, SCI, and/or 30-day death was then chosen for logistic regression analysis. The best subset of predictors was obtained via model reduction using the Akaike Information Criterion. Bootstrapping 5000 iterations was used for model validation.
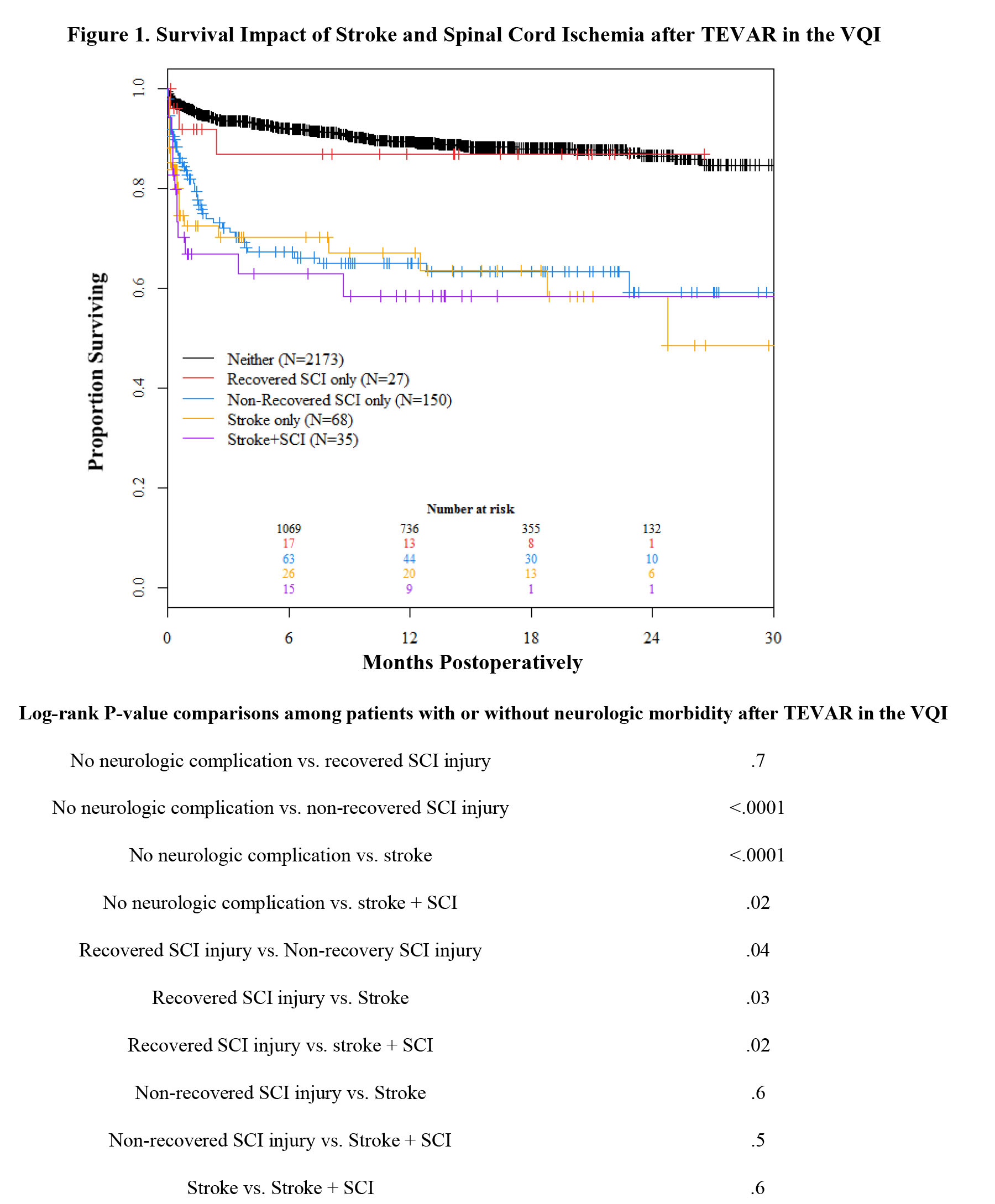
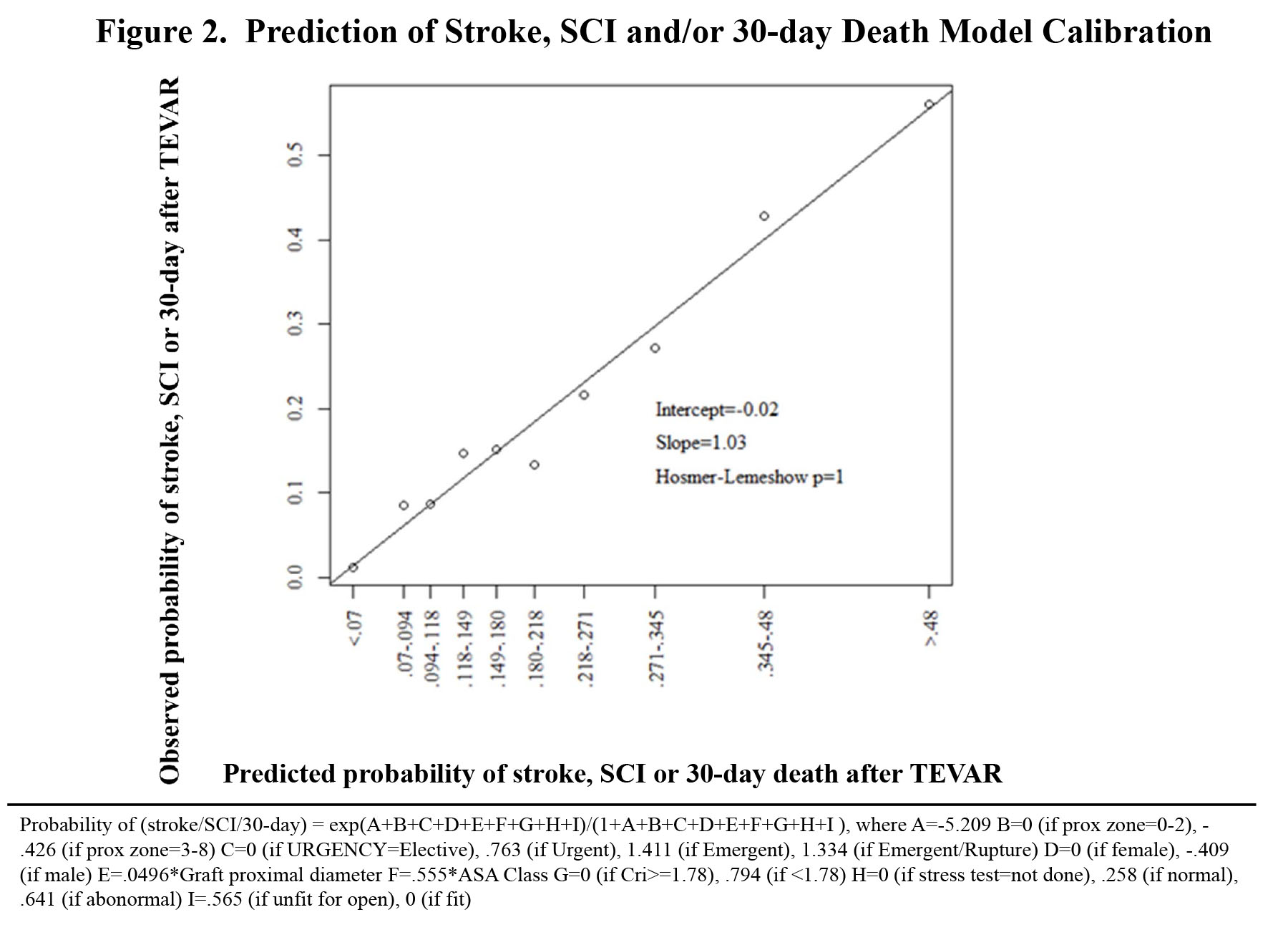
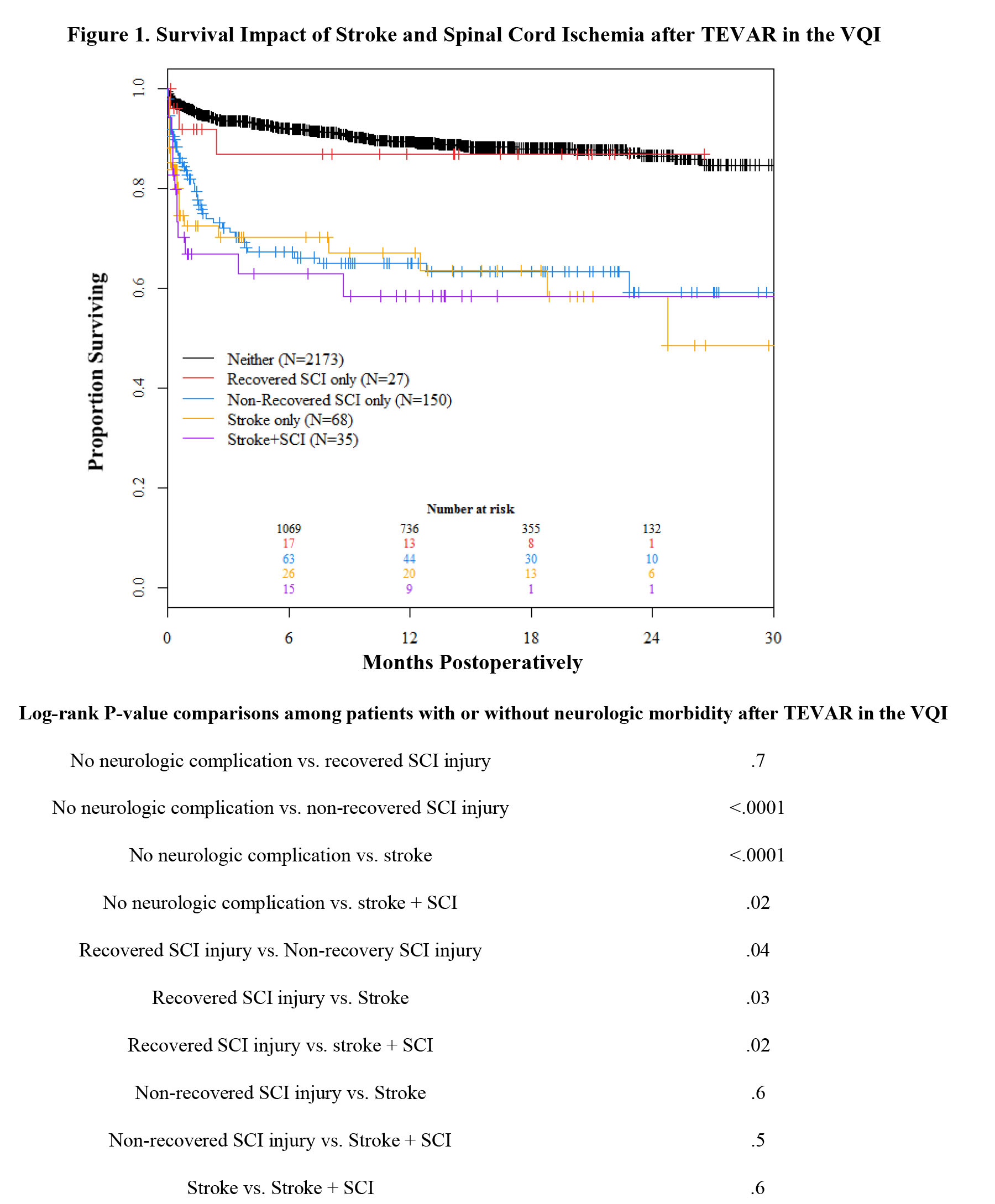
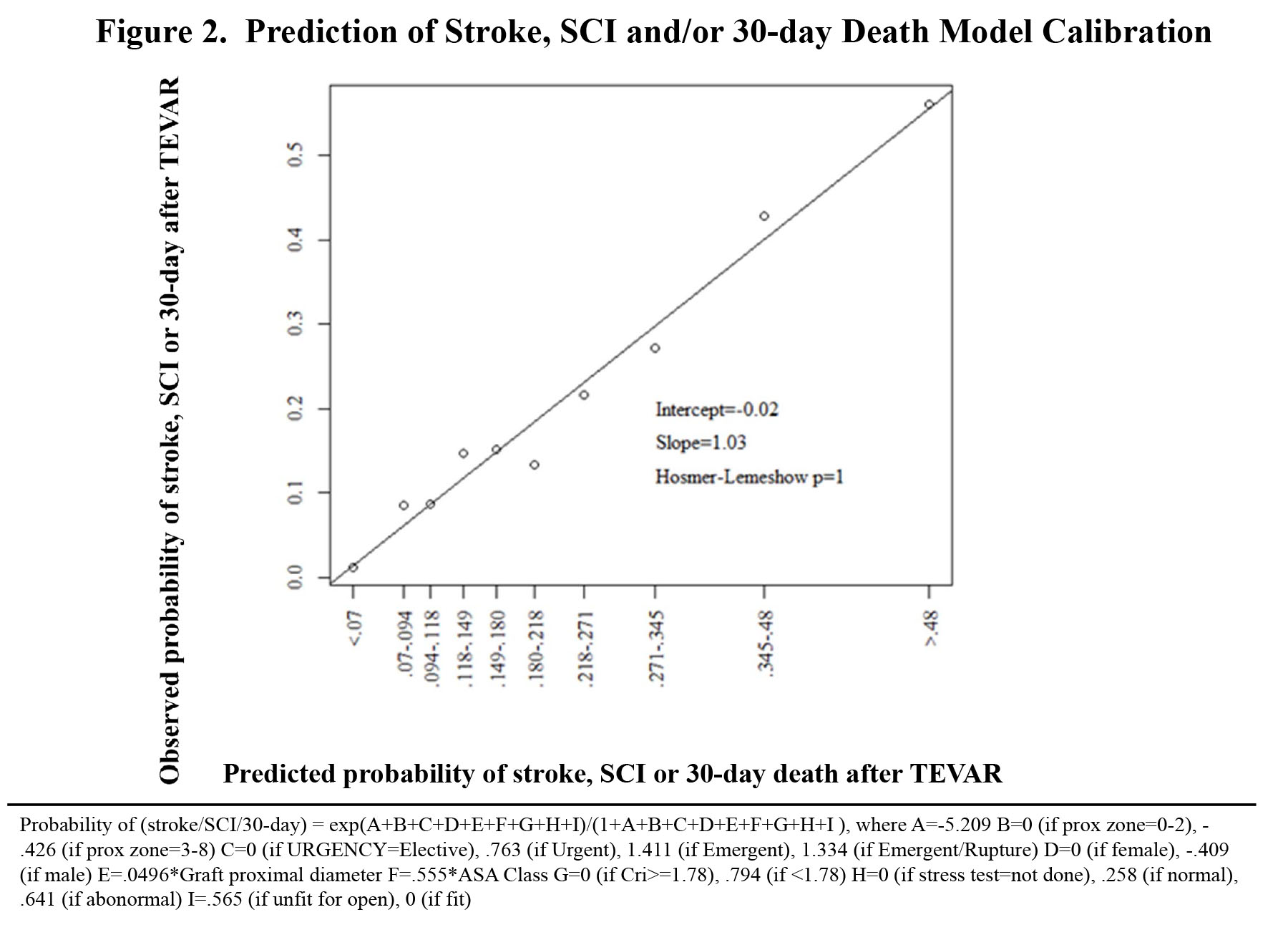
RESULTS: There were 2542 TEVAR procedures analyzed and the rate of any stroke, SCI and 30-day death were, respectively: 4.2% (N=103), 8.6% (N=231), and 8.4% (N=213). The impact on survival of SCI and/or stroke after TEVAR is illustrated in the Figure 1. Independent predictors of the composite endpoint(stroke/SCI/30-day death) included: ASA class OR multiplies 1.7 each unit increase(95% CI 1.4-2.1;P<.0001), emergent/rupture indication OR 4.1 (2.7-6.1;P<.0001), preoperative creatinine > 1.8 mg/dL OR 2.2 (1.5-3.3;P<.0001), deemed unfit for open repair OR 1.8 (1.4-2.2;P<.0001), abnormal preoperative stress test OR 1.5 (.7-3.1;P=.3), proximal landing zone 0-2 OR 1.5 (1.3-2;P<.0001), proximal graft diameter OR multiplies 1.05/mm (1.02-1.08;P<.0001, and female gender OR 1.5 (1.3-1.9;P=.001). The generalized estimating equations logistic regression with these chosen predictors had an area under the curve (AUC) = .759. In 5,000 boot strap runs, the mean model AUC = .759 (95% CI .730, .787) which demonstrates excellent discrimination and calibration(Figure 2).
CONCLUSIONS: Avoidance of stroke, SCI and/or 30-day death after TEVAR is tantamount to overall procedural success. Several simple predictors are identified that can preoperatively risk stratify patients for these potentially devastating outcomes. Implementation of this risk assessment tool may identify patients who are best treated with prophylactic pharmacologic and/or spinal drainage interventions to mitigate risk of developing neurologic morbidity and/or death after TEVAR.
Back to 2016 Annual Symposium Abstacts
|