|
Back to 2016 Annual Symposium Abstacts
Outcomes of Brachiocephalic Chimney Techniques used during Thoracic Endovascular Aortic Repair
Igor Voskresensky, M.D., Salvatore T. Scali, M.D., Robert J. Feezor, M.D., Javairiah Fatima, M.D., Kristina A. Giles, M.D., Rosamaria Tricarico, M.S., Scott A. Berceli, M.D., Ph.D., Thomas S. Huber, M.D., Ph.D., Adam W. Beck, M.D..
University of Florida-Gainesville, Gainesville, FL, USA.
OBJECTIVES: Brachiocephalic “chimney”(BCC) stents can be used as an adjunct to thoracic endovascular aortic repair(TEVAR) to treat proximal aortic pathology. However, the current literature remains inconclusive about the role of this technology. Herein we describe our experience with BCC stents with TEVAR.
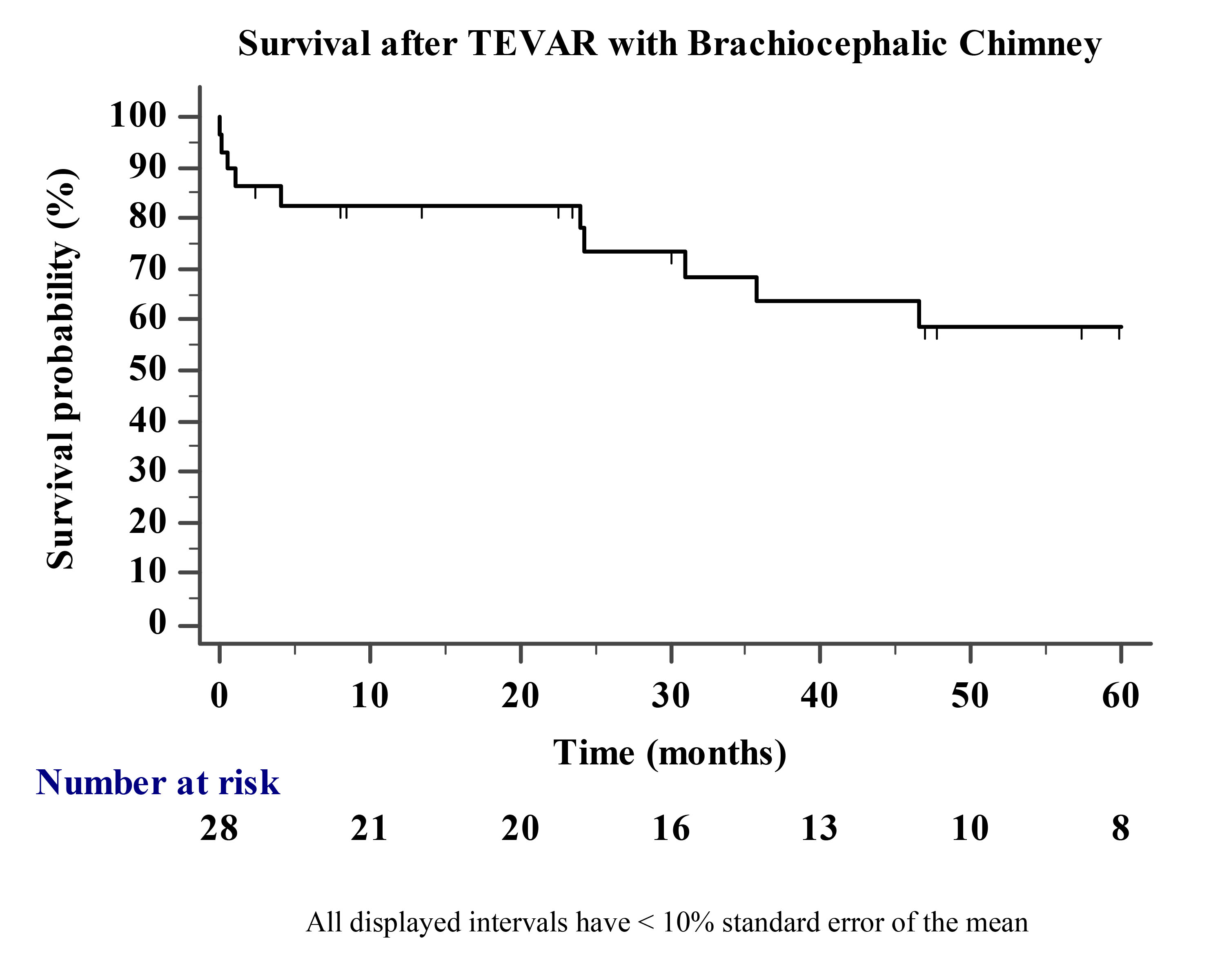
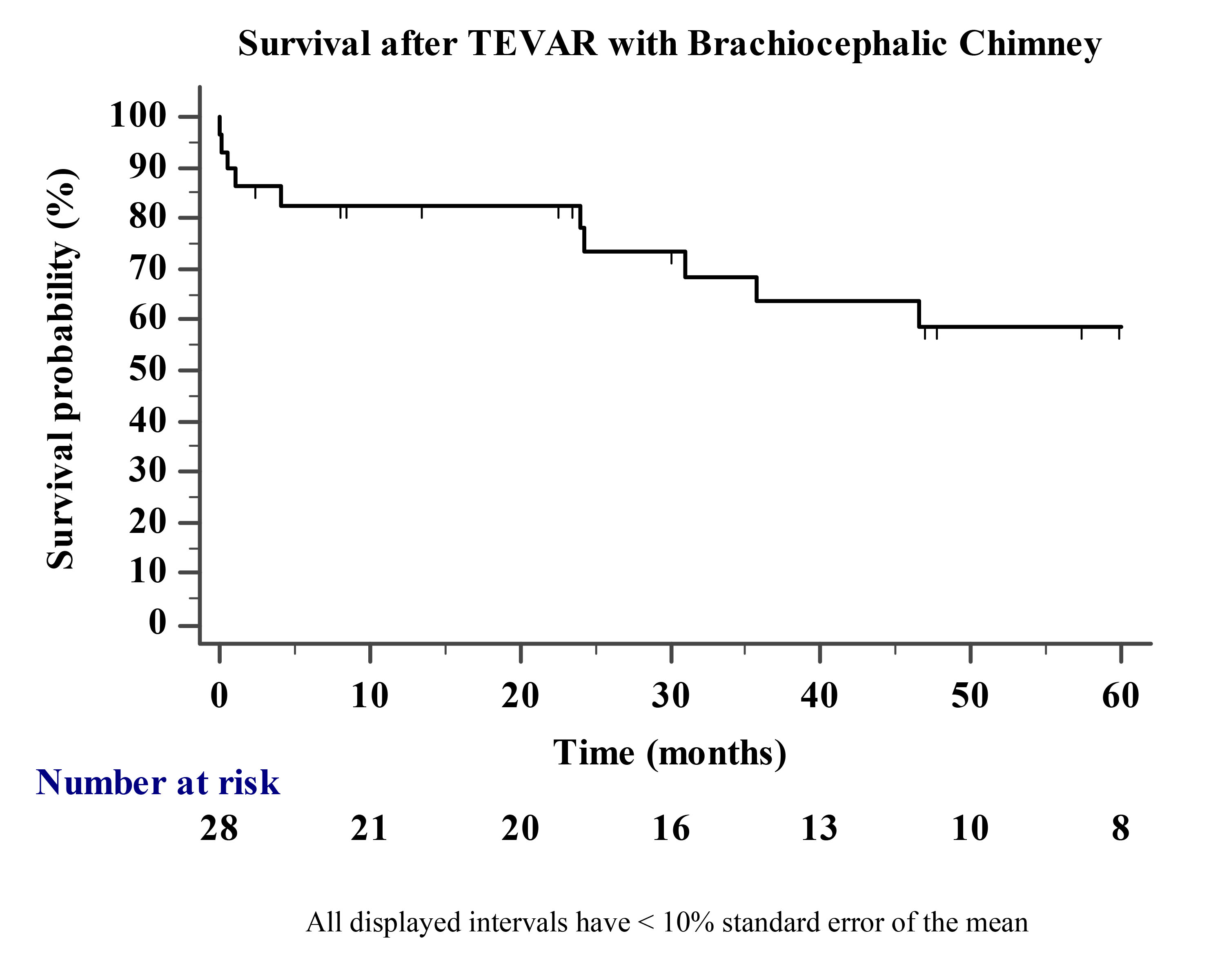
METHODS: All BCC TEVAR procedures from 2002-2015 were reviewed. Primary endpoints were 30-day and 1-year survival. Secondary endpoints included complications, reintervention, and endoleaks. Technical success was defined as BCC deployment at the intended treatment zone without type-1a endoleak in follow-up. The Kaplan-Meier method was used to estimate survival.
RESULTS: Twenty-nine patients[age-69±12 years(male-69%)] were identified. All were reported to be prohibitively high risk for open repair by a multidisciplinary team. Comorbidities included: CAD/MI(55%), CHF(14%), O2-dependent COPD(31%), and Cr>1.8mg/dL(17%). Presentations were: elective-18(62%), symptomatic-7(24%) and rupture-4(14%). Eleven(37%) had history of prior endovascular/open arch-descending-thoracic repair. Indications included degenerative aneurysm(N=13), chronic type-B dissection(N=4), type-1a endoleak(N=3), pseudoaneurysm(N=3), penetrating ulcer(N=3), acute type-B dissection(N=2), and blunt injury(N=1).
Thirty-four BC vessels were treated: innominate(N=8), left common carotid artery(CCA)(N=25), and left subclavian artery(N=1)[simultaneous innominate-LCCA, N=5(17%)]. BCC stents were planned in 69%(N=20) with the remainder placed for LCCA impingement(N=7) or residual type-1a endoleak requiring graft extension(N=2). Technical success was 90% and 28%(N=8) experienced an intraoperative complication(death-1, stroke-4[all unplanned BCCs], thromboembolism-1, subclavian artery repair-2).
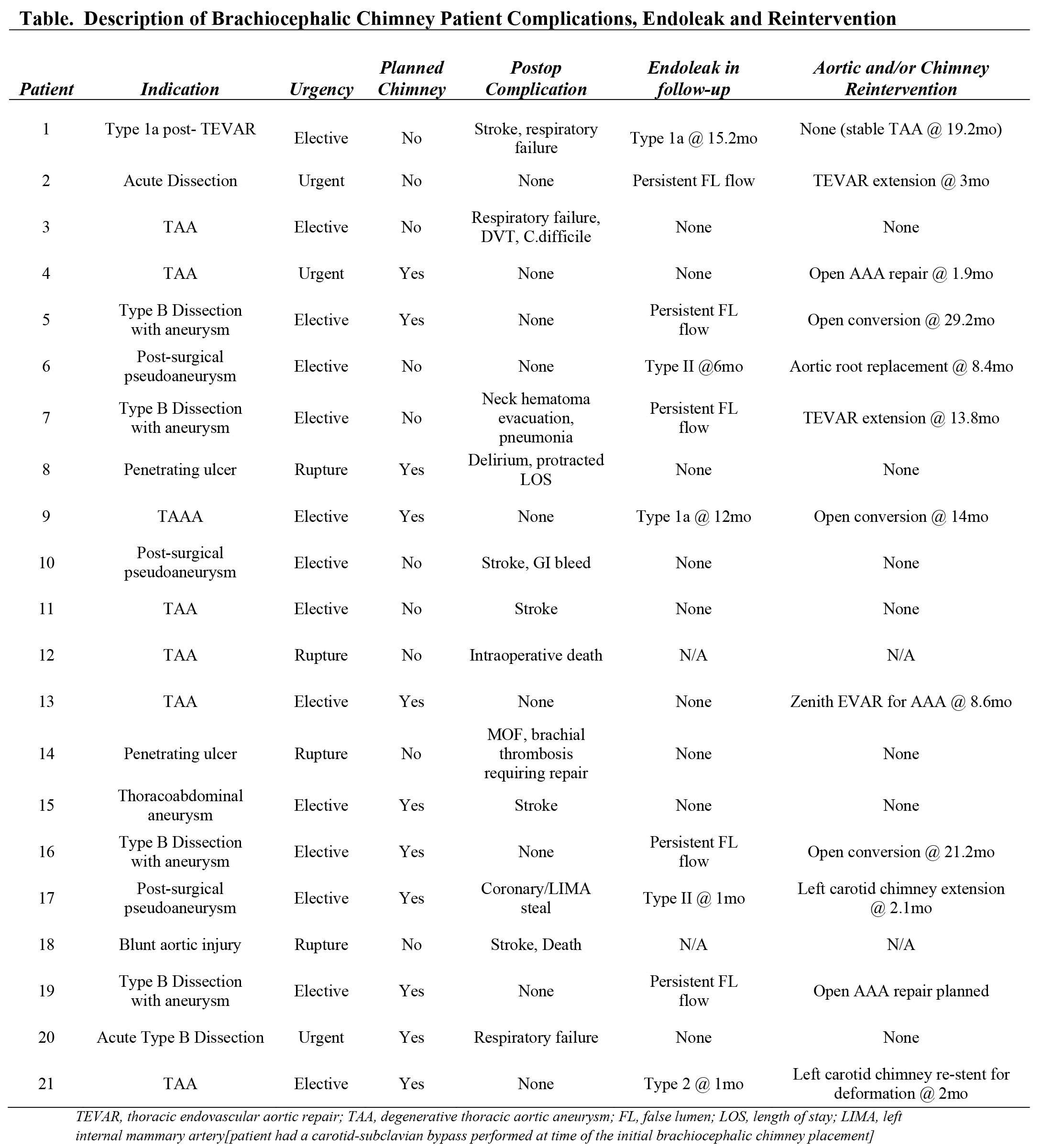
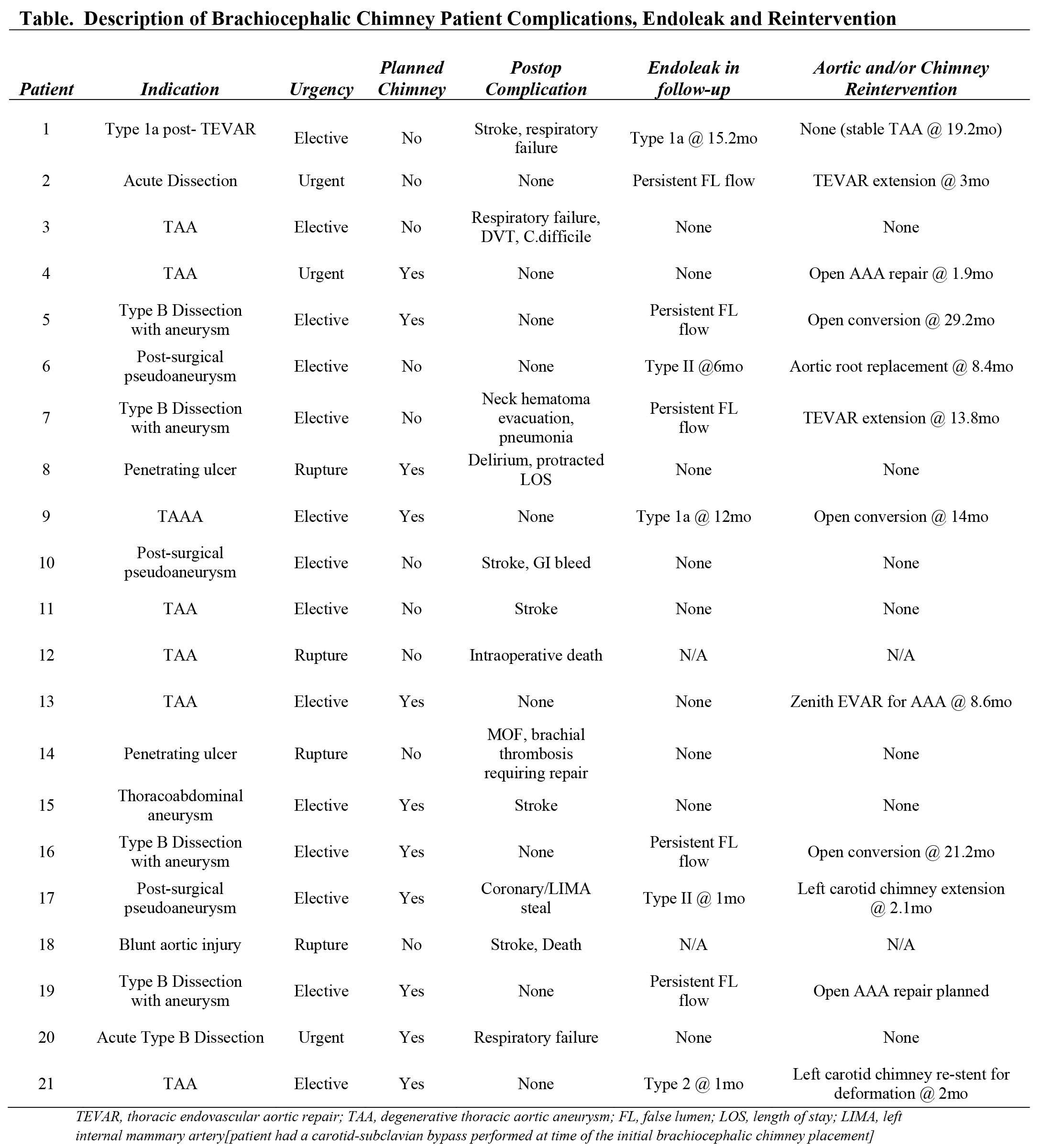
Thirty-day mortality was 7%[in-hospital-10%(N=3)]. Median LOS was 6 days[IQR 4, 9]. Major postoperative complications occurred in 38%(stroke 17%, SCI 0)(Table). Median follow-up was 6 months(IQR 1, 23). Nine(31%) patients underwent aortic-related reintervention and no chimney occlusions occurred during follow-up. Estimated one and 3-year survival is 82±7% and 65±9%, respectively(Figure).
CONCLUSIONS: BCC techniques are complex TEVAR adjuncts that can be completed with high technical success. However, perioperative morbidity is significant in these high-risk patients. Notably, unplanned BCC during TEVAR results in elevated stroke risk, but it is unclear if this was related to chimney placement or the inadvertent branch coverage that precipitated need for chimney salvage. Acceptable mid-term survival can be anticipated, but reintervention is not uncommon and vigilant follow-up is required.
Back to 2016 Annual Symposium Abstacts
|