Back to 2016 Karmody Posters
Dacron Patch Infection Following Remote History of Carotid Endarterectomy with Patch Angioplasty
Charles Hong, MD, Aleksandra Policha, MD, Caron B. Rockman, MD, Patrick J. Lamparello, MD.
Division of Vascular and Endovascular Surgery, New York University Langone Medical Center, New York, NY, USA.
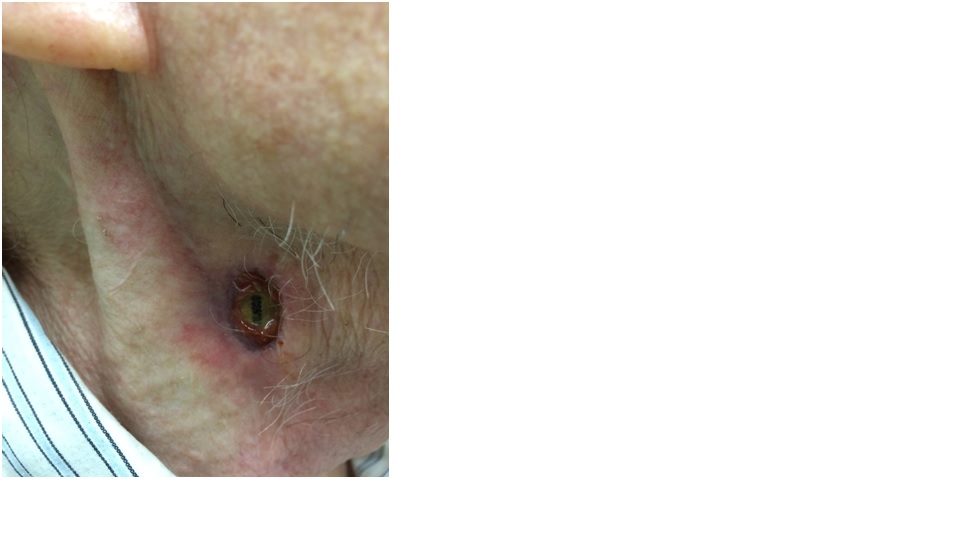
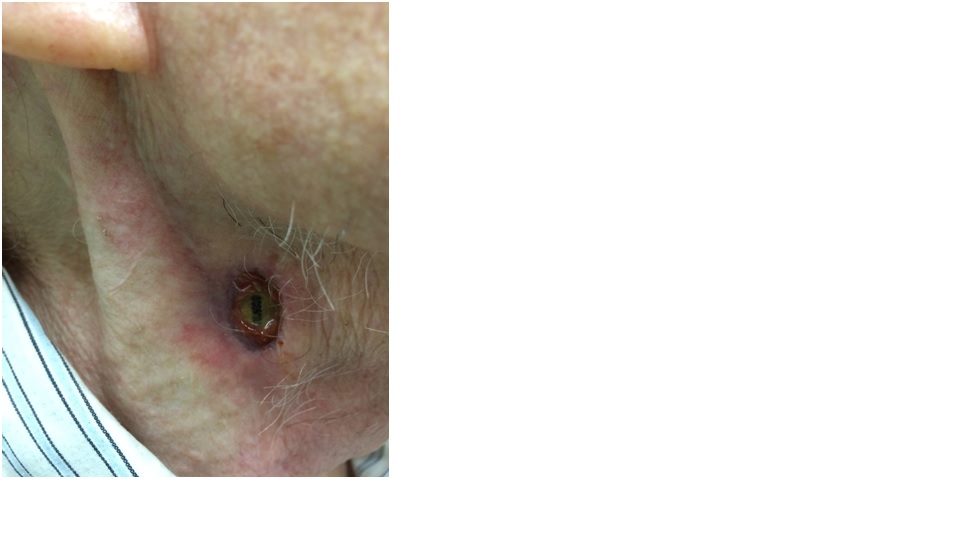
Objectives: Patch infection is a rare but serious complication of carotid endarterectomy (CEA) with prosthetic patch angioplasty. Signs and symptoms are often subtle, but the diagnosis should be suspected when a pseudoaneurysm is identified on imaging or when physical exam reveals a nonhealing wound, draining sinus, or localized swelling.
Methods: A 79-year-old man with a history of multiple dermatologic malignancies of the head and neck requiring minor interventions presented to an Otolaryngologist for a "non-healing neck wound." Eight years prior to the current presentation, he underwent bilateral CEA for asymptomatic severe carotid stenosis. At the time, he received appropriate perioperative antibiotic prophylaxis and had no perioperative complications. On exam, at the current presentation, a draining sinus was apparent along the anterior border of the sternocleidomastoid with exposed Dacron patch at the base of the wound (Figure). He was neurologically intact with no symptoms of systemic infection, neck mass, or bleeding. Neck computed tomography angiography revealed bilateral internal carotid artery pseudoaneurysms, right measuring 9 x 18 mm with an obvious soft tissue defect. After initiation of broad spectrum antibiotics, the patient underwent resection of the affected carotid segment and reconstruction with a reversed great saphenous vein interposition graft from the common carotid to the internal carotid artery. The external carotid artery was ligated. Coverage of the wound was performed with a musculocutaneous pectoralis flap. The procedure was performed under general anesthesia with intraoperative evoked potential monitoring.
Results: The patient tolerated the procedure well and recovered without complications. Blood and intraoperative wound cultures showed no bacterial growth. Surgical pathology revealed foreign body granulomatous reaction with no evidence of acute inflammation or bacterial infection. He was discharged on post-operative day 4 on continued oral antibiotic suppression with trimethoprim/sulfamethoxazole with plans for intervention on the left internal carotid artery pseudoaneurysm after full recovery.
Conclusions: Following CEA with prosthetic patch angioplasty, close surveillance of any postoperative wound complication is key and one must maintain a high index of suspicion for underlying graft infection. We advocate for definitive management with patch explant and autologous venous reconstruction. Antibiotic management should be guided by culture data when available.
Back to 2016 Karmody Posters
|