|
Back to 2016 Karmody Posters
Trends in Adoption and Outcome of Endovascular Repair for Ruptured Thoracic Aortic Aneurysms
Klaas H. Ultee1, Sara L. Zettervall, MD, MPH1, Peter A. Soden, MD1, Sarah E. Deery, MD1, Katie E. Shean, MD1, Hence JM Verhagen, MD, PhD2, Marc L. Schermerhorn1.
1Beth Israel Deaconess Medical Center, Boston, MA, USA, 2Erasmus Medical Center, Rotterdam, Netherlands.
OBJECTIVES:
Endovascular repair (TEVAR) has become an alternative to open repair for the treatment of ruptured thoracic aortic aneurysms (rTAA). The aim of this study was to assess national trends in the utilization of TEVAR for the treatment of ruptured rTAA and determine its impact on perioperative outcomes.
METHODS:
Patients admitted with a ruptured thoracic aortic aneurysm between 1993 and 2012 were identified from the Nationwide Inpatient Sample (NIS). Patients were grouped in accordance with their treatment: TEVAR, open repair, or nonoperative treatment. The primary outcomes were treatment trends over time and in-hospital death. Secondary outcomes included perioperative complications and length of stay. Trend analyses were performed using the Cochran-Armitage test for trend, and adjusted mortality risks were established using multivariable logistic regression analysis.
RESULTS:
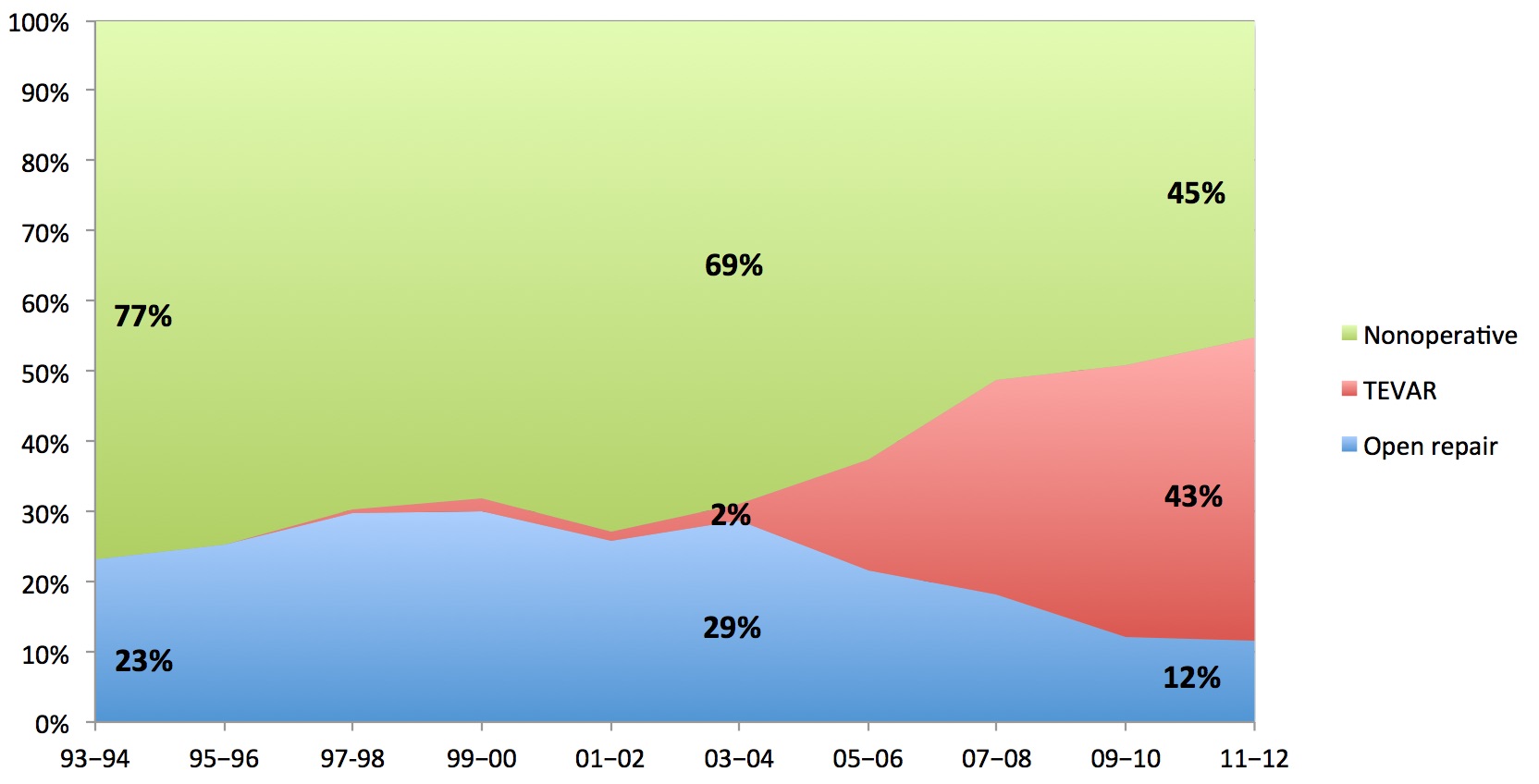
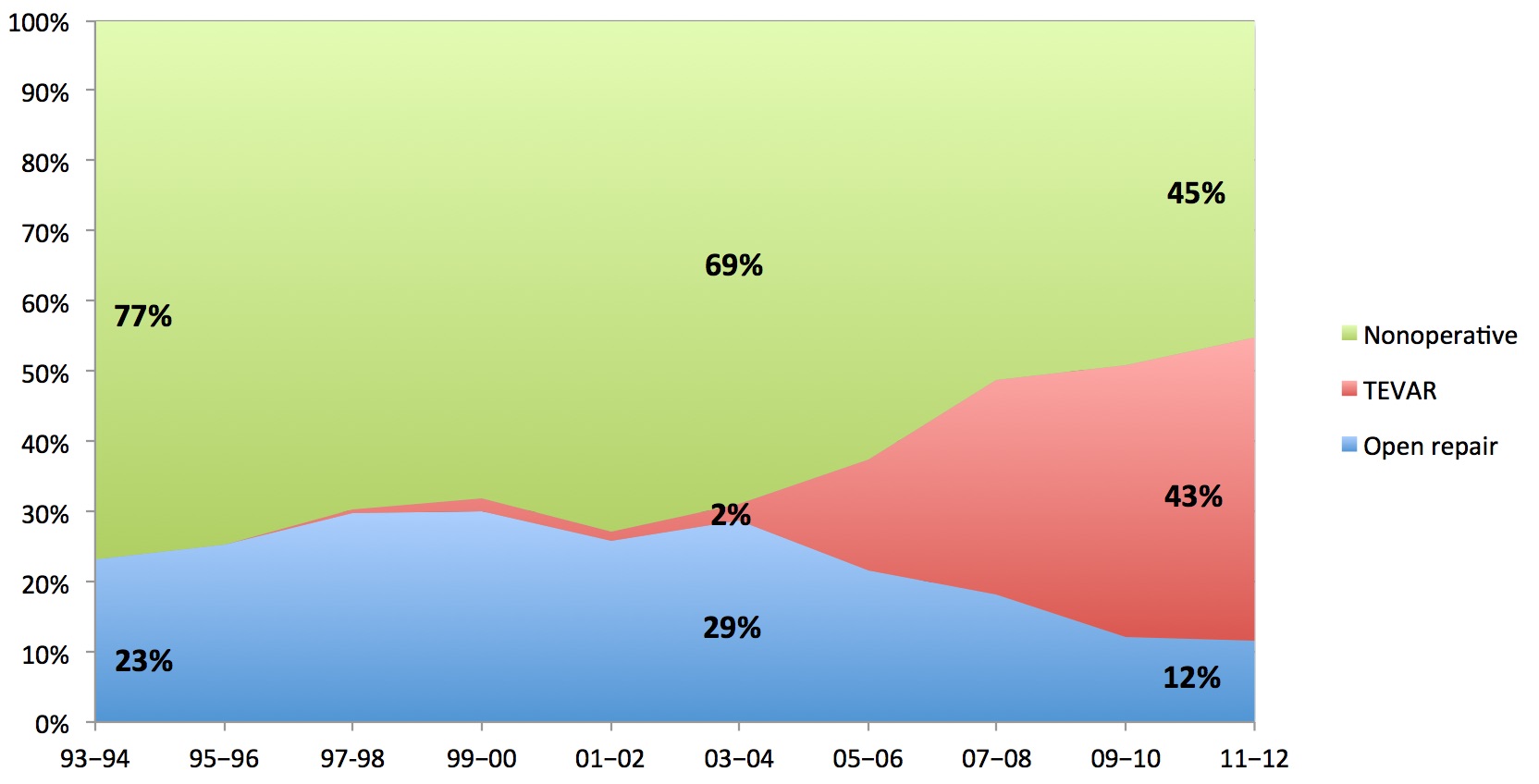
A total of 12,399 patients were included, with 1622 (13.1%) undergoing TEVAR, 2808 (22.6%) undergoing open repair, and 7969 (64.3%) not undergoing surgical treatment. TEVAR has been increasingly utilized from 2% in 2003-2004 of total admissions to 43% in 2012 (P<.001, Figure 1). Concurrently, the proportion of patients undergoing open repair declined from 29% to 12% (P<.001), and the proportion of patients treated nonoperatively from 69% to 45% (P<.001). Eligibility for surgical repair has increased for all age groups (P<.001 for all) since 1993-1994, but was most pronounced among those aged 80 years and with a 7.5 fold increase. After TEVAR was introduced, procedural mortality decreased from 48% to 27% (P<.001), while mortality among those undergoing no surgical treatment decreased from 64% to 60% (P<.001). Overall mortality following rTAA admission decreased from 60% to 42% (P<.001). Since 2005, mortality for open repair was 33.2% and 21.6% for TEVAR (P<.001). In adjusted analysis, open repair was associated with a two-fold higher mortality than TEVAR (OR: 2.0, 95% CI: 1.7 - 2.5).
CONCLUSIONS:
TEVAR has replaced open repair as primary surgical treatment for rTAA. The introduction of endovascular treatment has broadened treatment eligibility, particularly among the elderly. Mortality following rTAA admission has declined since the introduction of TEVAR, which is the result of improved operative mortality, as well as the increased proportion of patients undergoing surgical repair.
Back to 2016 Karmody Posters
|