|
Back to 2016 Karmody Posters
Retrograde Arch Extension in Acute Type B Aortic Dissection Does Not Affect Management and Outcomes
Foeke JH Nauta, MD1, Jip L. Tolenaar, MD, PhD2, Daniel G. Montgomery, BS3, Himanshu J. Patel, MD3, Jehangir J. Appoo, MD4, Nimesh D. Desai, MD5, Kim A. Eagle, MD3, Santi Trimarchi, MD, PhD1.
1Policlinico San Donato IRCCS, University of Milan, Milan, Italy, 2Thoracic Aortic Research Center, Policlinico San Donato IRCCS, Milan, Italy, 3University of Michigan, Ann Arbor, MI, USA, 4University of Calgary Medical Centre, Calgary, AB, Canada, 5University of Pennsylvania School of Medicine, Philadelphia, PA, USA.
Objective
Optimal treatment of acute type B aortic dissection with retrograde arch extension (RAE) remains undetermined. Our objective was to analyze the impact of RAE on management and outcomes in patients with a tear in the descending aorta.
Methods
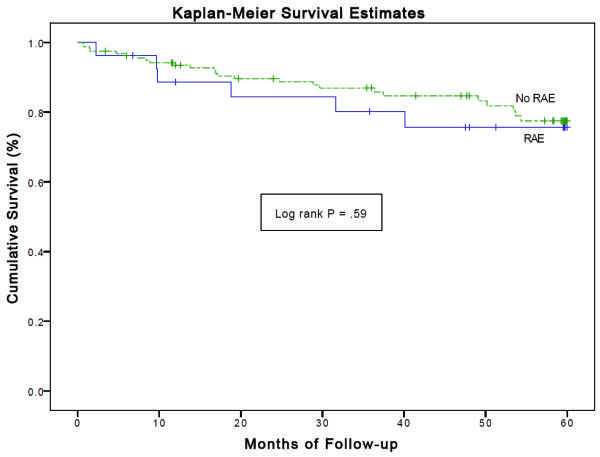
All acute type B dissection patients enrolled in IRAD between 1996 and 2014 were included. We found 337 (83.5%) patients with an entry tear in the descending aorta without RAE (dissection distal to the left subclavian artery, zone 3) and 67 (16.5%) with RAE (confined to the proximal or distal arch, zone 1 or 2). Kaplan-Meier survival curves were constructed and multivariate regression models were performed to identify independent predictors of RAE and follow-up mortality.
Results
Mean age was 63.3 ± 13.9 years and 65.7% was male. Independent predictors of RAE were partial false lumen thrombosis, large arch diameter, and small descending aortic diameter. Preoperative complications were more common among patients with RAE compared to those without RAE (67.2% vs 52.1%, P = .02). However, management strategies did not differ for patients with or without RAE, with 11.9% vs 9.5% open surgery (P = .54), 32.8% vs 31.1% endovascular repair (P = .78), 1.5% vs 3.0% hybrid approach (P = .70), and 53.7% vs 56.5% medical management (P = .68). In-hospital mortality was also similar for patients with (10.7%) and without RAE (10.4%, P = .96), and did not differ for open surgery (25.0% vs 0.0%, P = 0.17), endovascular repair (18.2% vs 8.6%, P = .24), hybrid approach (0.0% vs 10.0%, P = 1.00) and medical management (8.3% vs 9.4%, P = 1.00). Moreover, survival after 3- and 5-years was comparable for both entities (78.3% and 77.8% for RAE, and 88.2% and 84.4% for no RAE, log rank P = .27 and P = .59, respectively, Figure 1). Age ≥70 years and sharp pain at presentation were independently associated with 5-year mortality, RAE was not.
Conclusion
Acute type B dissection patients with RAE had similar management strategy and early and late mortality as those without RAE. This implies that patients with RAE seem not to benefit from a more aggressive approach. 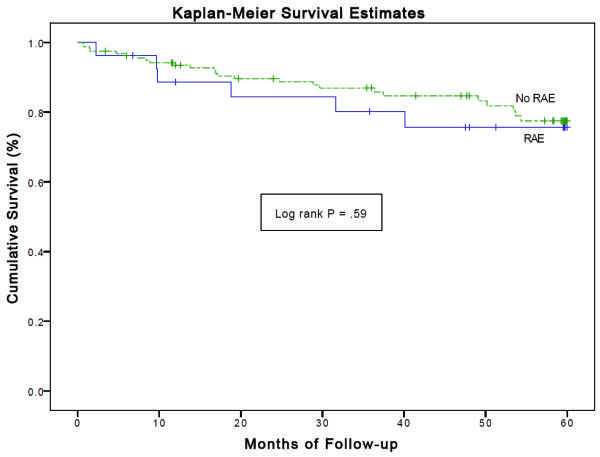
Back to 2016 Karmody Posters
|