|
Back to 2016 Annual Symposium Abstacts
Surgeon Leadership in the Coding, Billing, and Contractual Negotiations for Fenestrated Endovascular Aneurysm Repair (FEVAR) Increases Medical Center Contribution Margin and Physician Reimbursement.
Francesco A. Aiello, MD, Vijaya Daniel, M.D., Jonathan Durgin, BA, James Jenkins, BA, Louis Messina, MD, Daniel Doucet, MD, Jessica Simons, MD, Elias Arous, MD, Andres Schanzer, MD.
University of Massachusetts, Worcester, MA, USA.
OBJECTIVES:
Due to considerable device costs and increased procedure time, FEVAR is thought to result in financial losses for hospitals and physicians. We hypothesized that surgeon leadership in the coding, billing and contractual negotiations for FEVAR procedures increases hospital contribution margin and physician reimbursement.
METHODS:
At the UMASS Center for Complex Aortic Disease, a surgeon with expertise in medical finances is supported to manage the billing and coding of FEVAR procedures for hospital and physician reimbursement. A comprehensive financial analysis was performed for all FEVAR procedures (2011-2015), independent of insurance status or device utilization. Hospital contribution margin (CM; actual reimbursement-direct costs) was determined for each index FEVAR procedure and for all related subsequent procedures, inpatient or outpatient, 3-months prior and 1-year subsequent to FEVAR. CM for outpatient clinic visits, radiology exams, and vascular lab studies, related to FEVAR, were also determined. Surgeon reimbursement for FEVAR, related adjunct procedures, and assistant surgeon reimbursement were also calculated. All financial analyses were performed and adjudicated by the UMASS Department of Finance.
RESULTS:
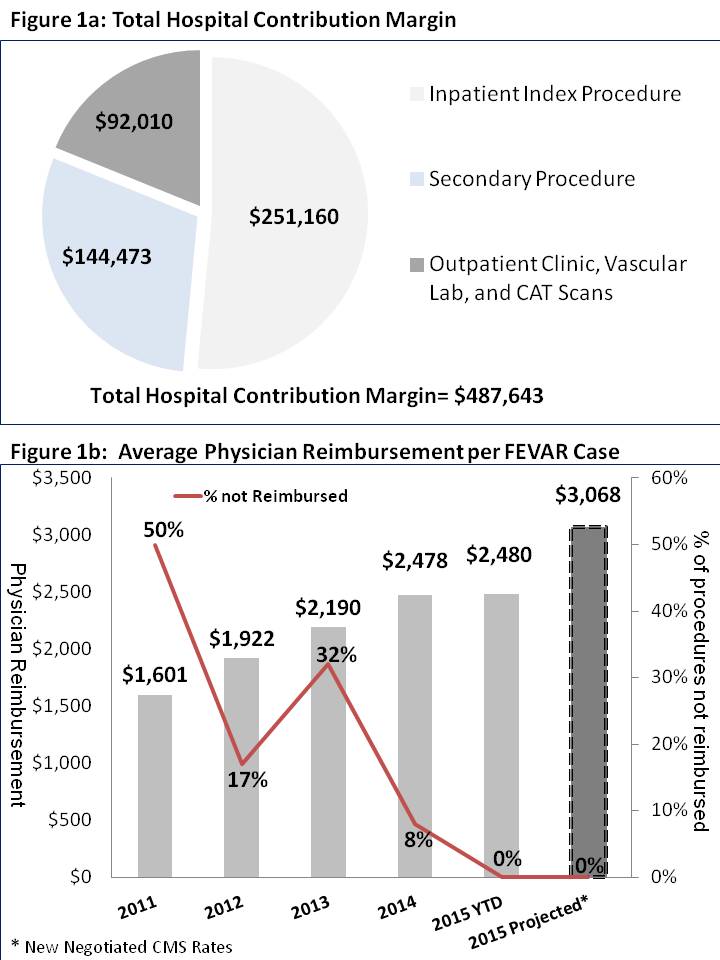
The index hospitalization for 63 FEVAR procedures generated \,027,887 of reimbursement, incurred \,776,726 of direct costs, resulting in a positive CM of \,160. Subsequent related hospital procedures(n=25) generated a CM of \,473. Outpatient clinic visits, radiologic exams and vascular lab studies generated an additional \,010 in revenue. Direct cost analysis revealed grafts accounted for the largest proportion of costs (55%), followed by supplies (12%), bed(12%), and OR(10%). Total medical center CM for all FEVAR services was \,643 (Figure 1a).
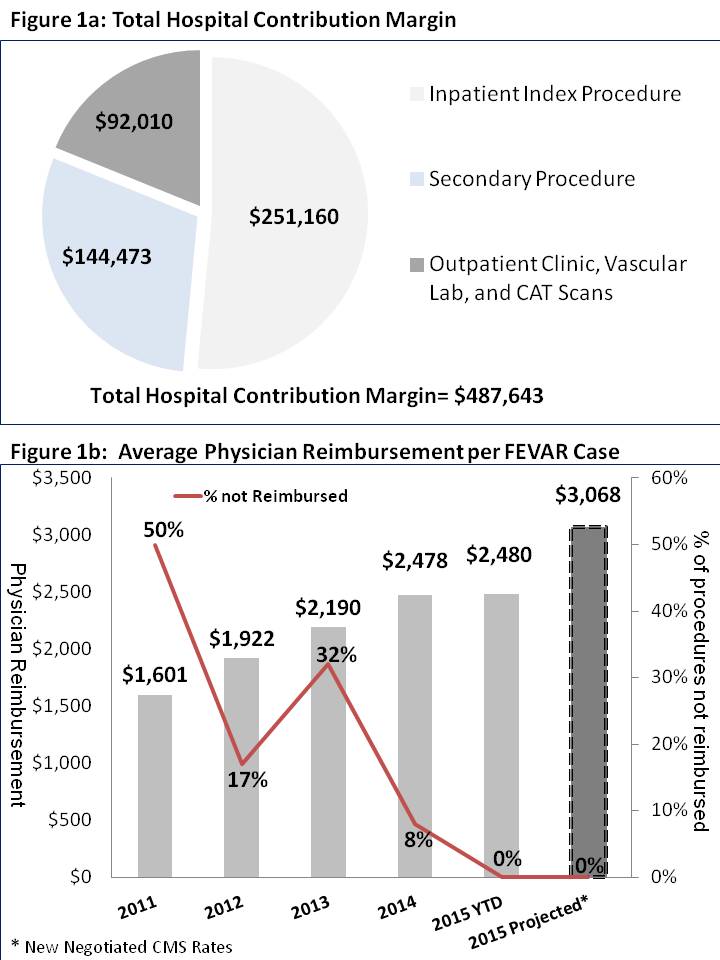
Average surgeon reimbursements per FEVAR from 2011 to 2015 increased from \,601 to \,480 while the surgeon payment denial rate declined from 50% to 0% (Figure 1b). Surgeon-led negotiations with CMS during 2015 resulted in a 27% increase in physician reimbursement for the remainder of 2015 (\,480 vs. \,068/case) and a 91% increase in reimbursement from 2011 (\,601vs. \,068). Assistant surgeon reimbursement also increased significantly (\ vs. \). Concomitant FEVAR related procedures generated an additional \,347 in surgeon reimbursement.
CONCLUSIONS:
Surgeon leadership in the coding, billing, and contractual negotiations for FEVAR results in a positive hospital contribution margin and increased physician reimbursement.
Back to 2016 Annual Symposium Abstacts
|