Back to 2016 Annual Symposium Abstacts
Evaluating Strategies for Reducing Scattered Radiation in Fixed-Imaging Operating Suites
Claire Miller, MS, Daniel Kendrick, MD, Andrew Shevitz, BS, Ann Kim, MD, Henry Baele, MD, David Jordan, PhD, Vikram Kashyap, MD.
University Hospitals - Case Medical Center, Cleveland, OH, USA.
OBJECTIVES:
High resolution fixed C-arm fluoroscopic systems allow for high quality endovascular imaging, but come at a cost of greater scatter radiation generation, and increased occupational exposure for surgeons. The purpose of this study is to evaluate the efficacy of two methods - a personal, real-time dose monitoring system and a dose reduction software algorithm - in reducing scattered radiation exposure.
METHODS:
A series of 158 cases were performed at a single institution over 16-months. Phase 1: Baseline radiation exposure was calculated. Phase 2: Staff used real-time radiation dose monitoring (dosimetry badges, Unfors RaySafe™). Phase 3: A software imaging algorithm was installed that reduces radiation (Philips EcoDose Software ™). All cases were performed in a fixed-imaging hybrid operating suite. Mean room dose and surgeon exposure (mSv) were compared during cases of varying complexity using unpaired t-test.
RESULTS:
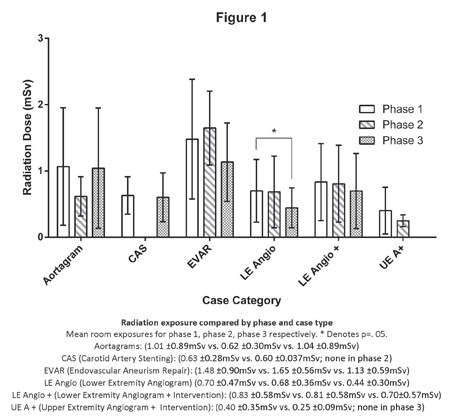
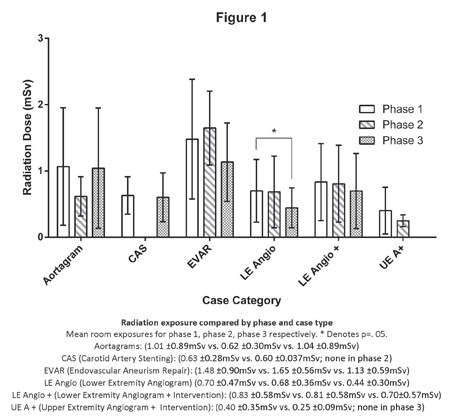
A total of 68 baseline cases, 34 cases in phase 2 and 56 cases in phase 3 were performed. Total mean surgeon dose varied across all case categories, with 46% and 32% dose reduction trends seen with real time exposure feedback during EVAR and upper extremity access cases respectively (Mean ±SD; 0.23 ±0.29mSv vs. 0.13 ±0.10mSv; 0.12 ±0.13mSv vs. 0.08 ±0.08mSv, p=NS). These cases involved the highest surgeon exposure at baseline. With the EcoDose software, reduction trends were seen in surgeon dose during CAS, EVAR and diagnostic lower extremity angiograms (Mean ±SD; 0.02 ±0.02mSv vs. 0.01 ±0.01mSv; 0.23 ±0.29mSv vs. 0.14 ±0.13mSv; 0.03 ±0.03mSv vs. 0.02 ±0.02mSv, p=NS). Total mean room dose was reduced in phase 3 when compared to baseline, (Figure 1) with diagnostic lower extremity angiograms showing significance (Mean ±SD; 0.70 ±0.47mSv vs. 0.44 ±0.30mSv, p=.053).
CONCLUSIONS:
Dose reduction software may be an effective technique to lower radiation exposure. However, real-time feedback of radiation exposure provides a negligible reduction because clinical needs supersede operative behavior changes. Implementation of strategies to reduce radiation is needed to reduce lifetime occupational radiation exposure for endovascular staff.
Back to 2016 Annual Symposium Abstacts
|